Cómo dominar el transporte de vacunas en cadena de frío 2025?
Actualizado el: 17 Noviembre 2025

Mantener la potencia de la vacuna requiere más que cámaras frigoríficas y cajas aisladas. En 2025, el mercado de logística de vacunas alcanzará aproximadamente Dólar estadounidense 3.29 mil millones, y la demanda sigue creciendo a medida que se amplían los nuevos programas de inmunización. Sin embargo, se estima 25–30% de las vacunas en el África subsahariana se pierden debido a las variaciones de temperatura. Esta guía muestra tú cómo construir una cadena de frío confiable para las vacunas, aprovechar las últimas tecnologías y cumplir con las regulaciones en evolución para garantizar que cada dosis llegue potente.
lo que define Transporte de vacunas en cadena de frío.? Descubra por qué son esenciales temperaturas constantes de 2 a 8 °C o temperaturas ultrafrías y cómo las desviaciones arruinan la potencia.
Cómo cumplir estrictos requisitos de temperatura? Descubra los rangos recomendados para las vacunas comunes, Fórmulas de ARNm y terapias celulares/génicas., junto con opciones de embalaje pasivas y activas.
¿Qué componentes componen la cadena de frío de una vacuna?? Entender las unidades de almacenamiento, sensores, Operadores y marcos de cumplimiento..
Cómo implementar una estrategia de logística de vacunas paso a paso? Siga un plan práctico que cubra la evaluación de riesgos., selección de equipos, planificación de ruta, seguimiento y planificación de contingencias.
¿Qué tendencias darán forma al transporte de vacunas en 2025? Explore innovaciones como unidades alimentadas por energía solar y entrega con drones, Optimización de rutas impulsada por IA y trazabilidad digital.
Preguntas frecuentes sobre el transporte de vacunas en cadena de frío.
¿Qué define el transporte de vacunas en cadena de frío??
Transporte de vacunas en cadena de frío se refiere al proceso de extremo a extremo de almacenar y mover vacunas mientras se mantiene un rango de temperatura constante. La mayoría de las vacunas convencionales deben permanecer entre 2 °C y 8 °C, mientras que las vacunas de ARNm como Pfizer BioNTech requieren –80 °C a –60 °C. Las desviaciones destruyen los ingredientes activos., lo que significa que cada paso, desde la fabricación hasta la entrega del último kilómetro, debe tener temperatura controlada.. La Organización Mundial de la Salud (OMS) estima que 25% de las vacunas en todo el mundo se dañan debido al mal funcionamiento de la cadena de frío, subrayando la importancia de sistemas robustos. Sólo en el África subsahariana, Energía poco confiable y causa de monitoreo limitado. 25–30% de pérdida de producto.
El transporte de vacunas en cadena de frío difiere del envío refrigerado general porque el fracaso de las vacunas socava directamente la salud pública.. Tu prioridad es preservar la potencia controlando la temperatura., exposición a la luz, humedad y manejo de golpes. Eso significa utilizar materiales de embalaje validados., dispositivos de monitoreo continuo, personal capacitado y planes de contingencia para retrasos.
Componentes de una cadena de frío para vacunas
Almacenamiento con temperatura controlada: Refrigeradores (2 °C-8 °C), congeladores (–50 °C a –15 °C), congeladores ultrabajos (–90 °C a –60 °C) y unidades criogénicas (< –80°C).
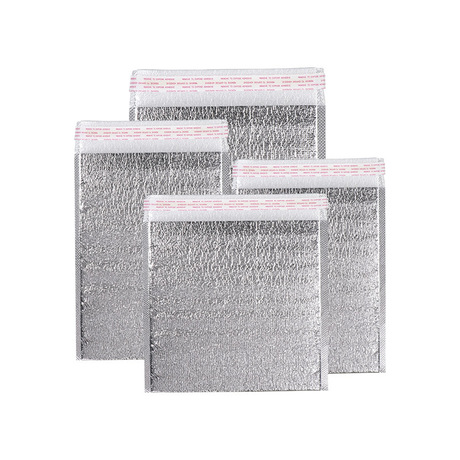
Sistemas de embalaje: Sistemas pasivos (cajas aisladas con bolsas de hielo o materiales de cambio de fase) y sistemas activos (Unidades de refrigeración motorizadas con control automático de temperatura.). Los sistemas pasivos son rentables para viajes cortos; Los contenedores activos manejan largas distancias y condiciones extremas..
Tecnología de monitoreo: Registradores de datos digitales, sensores de iot, GPS, Etiquetas RFID, y los paneles en la nube proporcionan la temperatura en tiempo real, datos de ubicación y shock. Los libros de contabilidad de Blockchain registran historiales de temperatura a prueba de manipulaciones.
Personal capacitado y SOP: El personal debe comprender los métodos de embalaje., interpretar las alertas de los sensores y documentar cada intervención. Procedimientos operativos estándar (Sops) definir responsabilidades, acciones de respuesta y requisitos regulatorios.
Cumplimiento regulatorio: El CDC, La OMS y la Ley de Seguridad de la Cadena de Suministro de Medicamentos (DSCSA) establecer reglas de almacenamiento y documentación. Por ejemplo, La DSCSA exige el intercambio de datos de transacciones electrónicas para rastrear productos farmacéuticos y prevenir la falsificación..
Cómo cumplir los estrictos requisitos de temperatura para las vacunas?
Rangos de temperatura recomendados
Las vacunas se dividen en varias categorías., cada uno con diferentes necesidades de temperatura. No seguir estos rangos puede hacer que una vacuna sea ineficaz o dañina:
| Rango de temperatura | Tipo de vacuna | Soluciones de embalaje | Importancia práctica |
| 2 °C – 8 °C | Vacunas estándar (sarampión, VPH, influenza); Agonistas del GLP 1 | Cajas refrigeradas con packs de gel, Materiales de cambio de fase, cargadores aislados | Mantiene la potencia para la mayoría de las vacunas de rutina.; recomendado por los CDC |
| –20 °C a –30 °C | Vacunas congeladas, vectores virales, algunos biológicos | Contenedores de hielo seco, unidades refrigeradas activas | Preserva la estabilidad del vector viral.; Requerido para ciertas dosis de polio y Ébola. |
| –80 °C a –60 °C | Vacunas de ARNm (p.ej., BioNTech de Pfizer), terapias génicas, terapias celulares | Congeladores ultrabajos, paneles aislados al vacío, Dewars de envío criogénicos | Esencial para la potencia del ARNm y la viabilidad celular.; un fallo puede destruir envíos enteros |
| < –80°C (criogénico) | Terapias celulares/génicas como CAR T; virus vivos atenuados | Transportadores secos de nitrógeno líquido, congeladores criogénicos | Mantiene la viabilidad de terapias regenerativas que requieren transporte a –150 °C. |
| Sala controlada (15 °C – 25 °C) | Vacunas orales, diluyentes, ciertos productos biológicos | Embalaje isotérmico con indicadores de temperatura. | Protege los productos sensibles tanto al calor como al frío. |
Mantener el rango correcto requiere un monitoreo continuo. Los CDC recomiendan utilizar registradores de datos digitales con sondas tamponadas para imitar los viales de vacunas y reducir las falsas alarmas. Para fórmulas de ARNm, una vez descongelados se pueden refrigerar a 2 °C–8 °C por hasta 10 semanas, pero no se deben volver a congelar. La fórmula de Moderna se puede conservar a –20 °C hasta su vencimiento y refrigerarse durante 60 días después de descongelar.
Opciones de embalaje
Embalaje pasivo utiliza cajas aisladas llenas de paquetes de gel, hielo seco o materiales de cambio de fase que absorben calor. Es adecuado para entregas de última milla y vuelos internacionales cortos.. Embalaje activo Incluye contenedores motorizados que mantienen temperaturas establecidas mediante compresores o unidades de refrigeración.; son ideales para recorridos largos, Viajes de varios días y condiciones extremas.. Materiales de cambio de fase (PCM) mantienen temperaturas precisas sin aporte de energía y, a menudo, se combinan con paneles aislados al vacío para envíos de ARNm. hielo seco (Co₂ sólido) puede mantener el contenido a –78,5 °C durante varios días, pero requiere ventilación para liberar gas; Las regulaciones limitan la cantidad permitida en los aviones..
¿Qué componentes componen la cadena de frío de una vacuna??
Equipos de almacenamiento y transporte.
Refrigeradores y congeladores: Las unidades básicas verticales o de pecho mantienen 2 °C–8 °C o –50 °C a –15 °C. Los modelos precalificados por la OMS incluyen refrigeradores que funcionan con energía solar para clínicas remotas.
Congeladores ultrabajos y criogénicos: Necesario para vacunas de ARNm y terapias celulares. Muchas instalaciones invierten en sistemas de energía de respaldo y monitoreo remoto para evitar fallas catastróficas..
Contenedores activos: Unidades accionadas por baterías o compresores utilizadas en aviones o camiones; Proporcionan un control preciso de la temperatura y reducen la dependencia del hielo seco..
Transportistas pasivos: Cajas isotérmicas con PCM o packs de gel. Son ligeros y rentables.; cuando se combina con embalajes validados y registradores de datos, Cumplen con muchos requisitos reglamentarios..
Modos de transporte: Aire (avión comercial o chárter), camino (camiones frigoríficos, furgonetas aisladas), mar (contenedores frigoríficos), y cada vez más drones para entregas remotas. El Se prevé que el mercado de servicios de entrega de drones médicos crezca desde USD 358.8 millones en 2025 a USD 2.5 mil millones por 2034, impulsado por la necesidad de una entrega e integración rápidas con IoT, IA y sistemas sanitarios remotos. Los drones entregan vacunas y muestras de laboratorio a zonas inaccesibles con retrasos mínimos.
Sistemas de seguimiento y trazabilidad
Registradores de datos: Proporcionar registro continuo de temperatura.. Registradores de datos digitales recomendado por la tienda CDC al menos 4,000 lecturas y tener memoria durante al menos dos años. Deben colocarse en el centro del embalaje y calibrarse anualmente..
sensores de iot: usar celular, Conectividad GPS o Bluetooth para transmitir la temperatura en tiempo real, datos de humedad y ubicación. Permiten alertas remotas si los parámetros se desvían de los rangos establecidos. La integración de IoT en los paquetes de vacunas proporciona una visibilidad sin precedentes y ayuda a reducir el desperdicio hasta en 50% según informes de la industria.
RFID y GPS: Las etiquetas RFID proporcionan seguimiento de ubicación y pueden activar actualizaciones automáticas cuando los contenedores pasan por los puntos de control.. Los rastreadores GPS agregan ubicación en tiempo real y pueden ayudar a planificar rutas alternativas durante retrasos.
cadena de bloques: Esta tecnología de contabilidad distribuida registra cada evento en la cadena de suministro., crear un historial de temperatura a prueba de manipulaciones. Plataformas como PharmaChain permiten a los reguladores y socios verificar la autenticidad y las condiciones de almacenamiento.. El FarmaAhora El informe señala que blockchain garantiza trazabilidad de extremo a extremo, mejora la confianza y reduce el fraude.
Procesos de soporte y cumplimiento
Procedimientos operativos estándar (Sops): Documentar cómo empacar envíos, cargar camiones, responder a excursiones y reportar datos. El personal debe seguir los POE para cada tipo de vacuna y mantener registros.
Programas de formación: El personal debe estar capacitado en embalaje., manejo, uso del registrador de datos, requisitos reglamentarios y procedimientos de emergencia. Los ejercicios de simulación ayudan a los equipos a practicar respuestas ante cortes o retrasos en el suministro eléctrico..
Marcos de cumplimiento: Las regulaciones clave incluyen buenas prácticas de distribución (PIB), Manual de gestión de vacunas de la OMS, Estados Unidos. Kit de herramientas de almacenamiento y manipulación de vacunas de los CDC y el DSCSA, que requiere datos de transacciones electrónicas y seguimiento digital para productos farmacéuticos. Los países pueden tener directrices nacionales como las de los CDC. 2025 recomendaciones para el mantenimiento de registros digitales.
Cómo implementar una estrategia de logística de vacunas paso a paso?
Siga este plan para diseñar y operar una cadena de frío de vacunas resiliente que minimice el desperdicio y cumpla con las expectativas regulatorias.:
Evaluar riesgos y cartera de vacunas: Identificar el rango de temperatura de cada vacuna y el tiempo de espera.. Determine cuáles requieren temperaturas ultrabajas o condiciones criogénicas.. Mapear riesgos potenciales, como largos tiempos de tránsito, acceso de última milla y cortes de energía.
Elija el embalaje adecuado: Según el rango de temperatura y la duración del envío, decidir entre sistemas pasivos o activos. Para envíos de 2 a 8 °C, Las cajas aisladas con paquetes de gel pueden ser suficientes.. Para envíos de ARNm, seleccione transportistas aislados al vacío y hielo seco o contenedores activos.
Validar equipo: Asegúrese de que todos los refrigeradores, Los congeladores y sensores están calibrados y certificados.. Realice pruebas para validar combinaciones de embalaje y medir la estabilidad de la temperatura durante el tiempo de viaje previsto..
Planificar rutas y transportistas: Elija transportistas con capacidades de cadena de frío validadas. Evaluar opciones de ruta para minimizar el tiempo de tránsito y evitar condiciones climáticas extremas.. Utilice análisis predictivos e inteligencia artificial para optimizar rutas; La IA puede reducir el tiempo de tránsito hasta 30%, según estudios de casos de la industria.
Implementar un monitoreo continuo: Equipe cada envío con sensores IoT y registradores de datos. Establecer umbrales de alerta y configurar notificaciones (correo electrónico, SMS) para desviaciones. Utilice paneles para rastrear envíos en tiempo real.
Preparar planes de contingencia: Desarrollar planes de respaldo para retrasos o fallas de equipos.. Por ejemplo, organizar previamente el acceso a instalaciones de refrigeración alternativas o suministros de hielo seco de emergencia. Capacite al personal sobre cómo responder a las alertas y documentar las acciones correctivas..
Mantener la documentación y el cumplimiento.: Registro de registros de temperatura, tiempos de entrega, e información de cadena de custodia. Utilice blockchain o registros digitales para garantizar la autenticidad. Cumplir con los requisitos de DSCSA para informes de transacciones electrónicas. Realizar auditorías periódicas y adaptar los POE a medida que evolucionan las regulaciones..
Revisar y mejorar: Después de cada envío, Revisar métricas de rendimiento como la estabilidad de la temperatura., tiempos de tránsito y respuestas a incidentes. Utilice análisis de datos para identificar patrones e implementar mejoras.. Relacionarse con socios externos para compartir las mejores prácticas y actualizar la capacitación..
Consejos para escenarios específicos
Clínicas remotas con energía poco confiable: Desplegar refrigeradores con energía solar equipado con monitoreo en tiempo real basado en sensores. Utilice vacunas con una vida útil más larga y capacite al personal para empacar los envíos rápidamente para reducir la exposición ambiental..
Entrega de última milla a zonas rurales: Usar transporte de drones Integrado con embalaje con temperatura controlada.. Los primeros resultados en Ruanda Modelo VaccAir demuestran que los drones reducen la pérdida de productos y mejoran los plazos de entrega.
Envíos de terapia celular de alto valor: Utilice recipientes dewar de nitrógeno líquido criogénicos con envases que absorban los impactos.. Incluir sensores redundantes para monitorear tanto el interior como el exterior del contenedor.. Organizar servicios de escolta para reducir los riesgos de seguridad..
Contingencia por falla del congelador: Mantenga generadores de repuesto o baterías de respaldo en el sitio. Si un congelador se calienta por encima de su umbral, transferir las vacunas a una unidad alternativa y marcar el lote para su evaluación. Utilice alertas digitales para notificar al personal y registrar acciones correctivas..
Caso del mundo real: En una clínica utilizando los sensores ColdTrace de Nexleaf, un corte de energía desencadenó una alerta que permitió al personal restaurar la refrigeración antes de que las temperaturas de las vacunas excedieran los límites seguros, ahorrando casi 2,000 dosis. Este ejemplo muestra cómo el monitoreo continuo previene pérdidas y garantiza la salud de la comunidad..
¿Qué tendencias darán forma al transporte de vacunas en 2025?
El panorama de la cadena de frío de las vacunas está evolucionando rápidamente. Mantenerse a la vanguardia significa comprender las fuerzas que definirán 2025 y más allá.
1. Digitalización y trazabilidad
sensores de iot, Las plataformas en la nube y blockchain brindan visibilidad de extremo a extremo.. Los registradores de datos en tiempo real y las etiquetas RFID envían la temperatura, lecturas de humedad y ubicación en tableros, permitiendo intervenciones proactivas. Blockchain garantiza registros de temperatura a prueba de manipulaciones, custodia y autenticidad.
2. Innovación en temperaturas ultrabajas
El auge de las vacunas de ARNm y las terapias génicas aumenta la demanda de equipos criogénicos. Los congeladores ultrabajos y los transportistas secos deben mantener entre –80 °C y –150 °C y, al mismo tiempo, reducir el uso de energía.. Los fabricantes están desarrollando sistemas con mejor aislamiento y respaldo de batería para soportar el transporte remoto. Muchos productos biológicos requieren logística criogénica, algunos productos necesitan transporte a –150 °C.
3. Drones y automatización de última milla
El El mercado de servicios de entrega de drones médicos crecerá desde USD 358.8 millones en 2025 a USD 2.5 mil millones por 2034. Los drones reducen los tiempos de entrega, Evitar el tráfico y llegar a lugares remotos.. Programas como VaccAir de Ruanda integran el transporte con drones con embalajes aislados para reducir la pérdida de productos. La automatización va más allá de los drones; Los sistemas automatizados de almacenamiento y recuperación en los almacenes reducen los errores de manipulación y permiten 24/7 operaciones.
4. Embalajes sostenibles y energías renovables
Los envases reutilizables y reciclables reducen los residuos y las emisiones de carbono. El Mercado de envases reutilizables para cadena de frío. se espera que crezca de Dólar estadounidense 4.97 mil millones en 2025 a USD 9.13 mil millones por 2034, impulsado por objetivos de sostenibilidad y el aumento de los envíos farmacéuticos. Los refrigeradores que funcionan con energía solar y los congeladores integrados con baterías reducen los costos de electricidad y apoyan a las zonas rurales. Las empresas invierten en camiones frigoríficos eléctricos y sistemas de seguimiento de la huella de carbono.
5. IA y análisis predictivo
La inteligencia artificial ayuda a pronosticar la demanda, optimizar rutas y predecir fallas de equipos. La IA puede analizar patrones climáticos, datos de tráfico e inventario para programar envíos, Reducir el tiempo de tránsito y el uso de energía.. El mantenimiento predictivo utiliza datos de sensores para detectar cuándo los congeladores necesitan servicio, evitando variaciones de temperatura.
6. Integración de One Health e innovaciones regionales
de África Una salud Las iniciativas integran las cadenas de suministro de vacunas para humanos y animales., compartir infraestructura energética y rutas de transporte para reducir costos y emisiones. El centro ACES en Ruanda utiliza energía solar, Unidades equipadas con sensores y transporte con drones para modernizar la distribución de vacunas.. La integración de la logística de vacunas para enfermedades zoonóticas con los programas de salud humana crea resiliencia y apoya la preparación para una pandemia..
7. Evolución regulatoria
Los reguladores están intensificando la supervisión del control de la temperatura, trazabilidad e integridad de datos. La DSCSA exige el intercambio electrónico de datos, mientras que los CDC enfatizan los registradores de datos digitales con sondas amortiguadas. La OMS y las agencias nacionales de salud están actualizando directrices para apoyar las terapias genéticas y de ARNm. Los marcos regulatorios seguirán evolucionando, exigir a las organizaciones que inviertan en formación, sistemas de calidad y tecnologías de cumplimiento.
Perspectivas del mercado y perspectivas regionales
Comprender el mercado ayuda a determinar las prioridades de inversión y el posicionamiento competitivo..
Tamaño del mercado de logística de vacunas: El mercado de logística de vacunas está valorado en Dólar estadounidense 3.29 mil millones en 2025 y se prevé que alcance Dólar estadounidense 4.25 mil millones por 2030, creciendo en un CAGR de 5.24%. Asia Pacífico es la región de más rápido crecimiento debido a la ampliación de los programas de inmunización, mientras que Europa posee actualmente la mayor proporción.
Mercado de almacenamiento y envasado de vacunas: Valorado en Dólar estadounidense 4.78 mil millones en 2024, Se prevé que este sector llegar a USD 8.11 mil millones por 2030 (CAGR ~9,1%). Los impulsores del crecimiento incluyen las vacunas de ARNm, Logística de temperatura ultrabaja y monitoreo digital.. Los EE. UU.. lidera el mercado con Dólar estadounidense 2.27 mil millones en 2024.
Mercado de envases reutilizables: Los envases reutilizables para la cadena de frío crecerán a partir de Dólar estadounidense 4.97 mil millones en 2025 a USD 9.13 mil millones por 2034, Reflejando las demandas de sostenibilidad y ahorro de costos.. Los sistemas reutilizables a menudo integran seguimiento de IoT y paneles aislados al vacío..
Mercado de entrega de drones: El mercado de servicios de entrega de drones médicos se expandirá desde Dólar estadounidense 358.8 millones en 2025 a Dólar estadounidense 2.5 mil millones por 2034, representando un CAGR de 24.1%.
Logística de cadena de frío para productos biológicos: Acerca de 85% de los productos biológicos requieren control de temperatura, y casi 50% de las vacunas se desperdician en todo el mundo debido a una mala gestión de la cadena de frío. La logística criogénica se mantiene aproximadamente 31.45% de la cuota de mercado y se espera que se expandan debido al crecimiento de la terapia celular y genética.
Preguntas frecuentes
Q1: ¿Por qué es tan importante el control de la temperatura para las vacunas??
Las vacunas son productos biológicos que pierden potencia cuando se exponen al calor o al frío extremo.. Por ejemplo, Las vacunas de ARNm deben permanecer entre –80 °C y –60 °C; Incluso una breve exposición a la temperatura ambiente puede degradarlos.. El monitoreo continuo garantiza que las desviaciones se detecten y corrijan. Utilice registradores de datos digitales con sondas amortiguadas y responda inmediatamente a las alertas.
Q2: ¿Qué debo hacer si un envío de vacunas experimenta un aumento de temperatura??
Primero, separar el envío afectado y ponerlo en cuarentena. Recuperar registros de temperatura de los registradores de datos y determinar la duración y magnitud de la excursión.. Póngase en contacto con el fabricante de la vacuna o las autoridades sanitarias para obtener orientación.. No use ni deseche la vacuna hasta que reciba instrucciones.. Documentar el incidente e implementar acciones correctivas., como mejorar el embalaje o formar al personal.
Q3: ¿Cómo puedo reducir las emisiones de carbono en el transporte de vacunas??
Utilice envases reutilizables para reducir el desperdicio y elija transportistas que inviertan en vehículos energéticamente eficientes.. Opte por fuentes de energía renovables, como refrigeradores que funcionan con energía solar y camiones electrificados.. Planifique rutas utilizando IA para minimizar las millas recorridas. Participar en programas que compensen las emisiones de carbono a través de inversiones en energías renovables..
Q4: ¿Son seguros los drones para entregar vacunas??
Sí, cuando está adecuadamente diseñado y regulado. Los drones utilizados en la entrega de vacunas tienen compartimentos aislados para mantener la temperatura, GPS para una navegación precisa y sensores para monitorear las condiciones. Proyectos como VaccAir de Ruanda muestran que las entregas con drones pueden reducir la pérdida de productos y mejorar la puntualidad en las entregas.. Sin embargo, Requieren aprobación regulatoria y operadores capacitados..
Q5: ¿Qué papel juega blockchain en las cadenas de frío de las vacunas??
Blockchain proporciona una seguridad, Libro de contabilidad inmutable de cada evento en la cadena de suministro., incluyendo datos de temperatura, transferencias de custodia y cumplimiento normativo. Esta transparencia reduce el fraude., contrarresta las vacunas falsificadas y permite a los reguladores auditar los envíos rápidamente. Blockchain también simplifica la trazabilidad bajo regulaciones como DSCSA.
Resumen y recomendaciones
El transporte de vacunas en cadena de frío exige un control meticuloso de la temperatura, manejo y documentacion. El mercado de la logística de vacunas está creciendo, y el riesgo de pérdida de producto debido a variaciones de temperatura sigue siendo alto. Las conclusiones clave incluyen:
Mantener temperaturas correctas: Mantenga las vacunas estándar en 2 °C–8 °C y vacunas de ARNm de –80 °C a –60 °C. Utilice envases activos o pasivos que coincidan con los requisitos de cada vacuna y considere contenedores criogénicos para terapias avanzadas..
Implementar un monitoreo continuo: Utilice registradores de datos digitales, Sensores de IoT y blockchain para visibilidad y trazabilidad en tiempo real. Responda rápidamente a las alertas para evitar daños.
Planificar proactivamente: Evaluar riesgos, validar equipo, optimizar rutas y preparar planes de contingencia. Capacite al personal sobre los SOP y los requisitos de cumplimiento, como la DSCSA..
Adoptar tecnologías sostenibles e innovadoras: Mejor drones para entregas de última milla, Refrigeración con energía solar y embalajes reutilizables.. Integre IA y análisis predictivo para optimizar las operaciones.
Fortalecer la colaboración de One Health: Coordinar las cadenas de suministro de vacunas para humanos y animales para mejorar la eficiencia y la resiliencia..
Siguiendo estas recomendaciones y manteniéndose informado sobre tecnologías y regulaciones emergentes, se puede construir una cadena de frío resiliente que proteja la potencia de la vacuna y respalde los objetivos mundiales de inmunización.
Acerca de Tempk
En Templ, Nos especializamos en soluciones logísticas de temperatura controlada para vacunas y productos biológicos.. Nuestro equipo combina décadas de experiencia en cadena de frío con tecnología de vanguardia.. Ofrecemos sistemas de embalaje validados, refrigeradores con energía solar, contenedores de envío equipados con registrador de datos y Paneles de monitoreo basados en la nube que cumplen o superan los requisitos de la OMS y DSCSA. Nuestras soluciones están diseñadas para ofrecer flexibilidad, permitiéndole escalar desde el transporte a nivel clínico hasta la distribución global. Trabajamos con clientes en el sector sanitario., investigación y salud pública para garantizar que sus vacunas lleguen potentes, seguro y a tiempo.
Llamado a la acción: Listo para mejorar la logística de sus vacunas? Contáctanos para una consulta personalizada. Nuestros expertos valorarán tus necesidades, recomendar el equipo adecuado y ayudarle a implementar un, cadena de frío preparada para el futuro.