Vaccine Cold Chain Standards: How to Protect Your Vaccines in 2025
Actualizado en noviembre 27, 2025
Proper vaccine cold chain standards keep vaccines safe from manufacturing to injection. En 2025 the market for vaccine shippers is forecast to grow from $1.5 billion to $3.5 mil millones por 2033. As immunization programs expand and new mRNA vaccines require ultra cold conditions, understanding how you manage the cold chain is critical. This guide uses simple language and real world examples to explain vaccine cold chain standards, including recommended temperature ranges, equipment selection, monitoring practices, staff training and the latest trends. You’ll see why these standards matter and how they help tú maintain vaccine potency.

What are the updated vaccine cold chain standards and why do they matter?
How should vaccines be stored – refrigerated, frozen or ultra cold?
Which refrigerators and freezers meet vaccine storage requirements?
How do you monitor temperature and respond to excursions?
What are the new trends and innovations in cold chain management?
How do you develop SOPs and train staff for emergency preparedness?
Why are vaccine cold chain standards important in 2025?
Cold chain standards preserve vaccine potency. Vaccines are biological products; exposure outside their prescribed temperature ranges degrades proteins and lipids. Most routine vaccines must stay between 2 °C y 8 °C (36 °F–46 °F). Live vaccines like varicella and some COVID 19 formulations require storage between –50 °C and –15 °C, while mRNA vaccines such as Pfizer BioNTech Comirnaty need ultra cold temperatures of –90 °C a –60 °C. Deviating from these standards can render vaccines ineffective, leading to wasted doses and revaccination.
Cold chain failures have real consequences. Imagine leaving a cake in the sun: essential ingredients break down and the cake spoils. Similarmente, overheating vaccines destroys fragile proteins, while freezing can form ice crystals that damage molecular structure. A community pharmacy in upstate New York once saved over US$20,000 worth of vaccines because staff had a backup unit and executed their emergency plan when a freezer failed. Without adherence to standards, those vaccines would have been lost.
Maintaining the cold chain is about more than equipment. It involves accurate inventory management, reliable storage and temperature monitoring, y well trained staff. As you read this guide, keep in mind that the purpose of standards is to protect patients, reduce waste and build trust in immunization programs.
What happens when cold chain standards are not followed?
Ignoring standards can cause vaccines to lose potency, leading to ineffective immunization and potential outbreaks. Temperatures outside the recommended range degrade active ingredients. Freezing certain vaccines can break emulsions or damage adjuvants, making the dose unusable. Even brief excursions may require discarding the vaccine, causing financial loss and delayed patient care. In regulatory terms, failure to comply can also result in penalties or loss of program eligibility.
| Storage Failure Scenario | Likely Impact | Lo que significa para ti |
| Refrigerator temperature rises above 8 °C for several hours | Vaccine potency decreases; doses must be discarded | Financial loss and revaccination; may delay patient care |
| Freezer drops below –50 °C | Temperature excursion may damage varicella or mRNA vaccines | Requires quarantine and stability consultation; potential waste |
| Use of dormitory style combination refrigerator/freezer | Uneven cooling; risk of freezing vaccines stored near the freezer plate | Not recommended for vaccines |
| Inadequate monitoring (no digital data logger) | Excursions go unnoticed; unknown duration of temperature breach | Puts all stored vaccines at risk and jeopardizes program compliance |
Practical advice and user tips
Keep vaccines between 2 °C y 8 °C, unless manufacturer guidelines specify otherwise.
Never use combination or dormitory style units; these are prone to temperature fluctuations.
Check temperatures twice daily and document min/max readings.
Use backup power and emergency plans to maintain storage during outages.
Train all staff on proper storage, monitoring and emergency procedures.
ejemplo real: During the early 2020s, a clinic stored vaccines in a dormitory refrigerator because of space constraints. When staff checked the next morning, temperatures had dipped to 1 °C and spiked to 12 °C. All vaccines had to be discarded. The clinic replaced the unit with a pharmaceutical grade refrigerator and implemented daily monitoring, preventing future losses.
What are the recommended temperature ranges for vaccine storage?
Different vaccines require specific temperature ranges. Knowing these ranges is the foundation of any vaccine cold chain program.
Refrigerated vaccines: 2 °C-8 °C
The majority of routine vaccines—such as influenza, DTaP, HPV and MMR—must be stored in a refrigerator between 2 °C y 8 °C (36 °F–46 °F). Keeping the thermostat at approximately 5 °C helps minimize fluctuations. Pharmaceutical grade or purpose built refrigerators are designed to maintain these temperatures uniformly and recover quickly after door openings.
To ensure stability:
Place vaccines in their original packaging to protect them from light and preserve lot information.
Store vaccines in the center of shelves, away from walls and door compartments.
Do not overcrowd; allow air to circulate and use water bottles to stabilize temperatures.
Vacunas congeladas: –50 °C a –15 °C
Varicella (chickenpox), some Mpox vaccines and certain COVID 19 formulations require freezer storage between –50 °C and –15 °C (–58 °F to 5 °F). Stand alone freezers are preferred; combination units risk exposing vaccines to warm air from the refrigerator compartment. Manual defrost units may need regular defrosting to prevent ice build up and maintain temperature uniformity.
When storing frozen vaccines:
Keep the digital data logger probe adjacent to vaccines in the central area.
Do not store food or beverages in vaccine freezers.
Use frozen water bottles as thermal ballast and for emergency transport.
Ultra cold vaccines: –90 °C a –60 °C
Vacunas de ARNm, including Pfizer BioNTech Comirnaty and other advanced biologics, require ultra cold storage between –90 °C y –60 °C. Ultra cold freezers have alarms, backups and specialized insulation. Notablemente, thawed Pfizer BioNTech vials can be stored in a refrigerator (2 °C-8 °C) a hasta 10 semanas; Moderna vaccines may be refrigerated for up to 30 días after thawing. Always follow manufacturer instructions and never refreeze thawed doses.
Monitoring and documentation requirements
Maintaining these temperature ranges requires continuous monitoring and thorough documentation:
Use calibrated digital data loggers (DDL). The CDC recommends DDLs with buffered probes, out of range alarms, low battery indicators and the ability to record min/max temperatures. NIST certified devices ensure accuracy and compliance.
Record temperatures at least twice daily—at the start and end of each workday—and review logs regularly.
Review and download data every two weeks and after any excursion. Keep documentation for at least three years to meet audit requirements.
Label vaccines “Do NOT Use” if an excursion occurs, separate them from other stock and contact your immunization program or manufacturer for guidance.
User tip: Place a sign on or near the refrigerator listing acceptable temperature ranges and emergency procedures. This quick reference helps your team respond swiftly to deviations.
How to choose the right cold chain equipment
Selecting the right equipment is vital for maintaining vaccine cold chain standards. Not all refrigerators and freezers perform equally; purpose built units undergo rigorous testing to keep vaccines within required ranges and recover quickly from door openings.
Pharmaceutical grade refrigerators and freezers
Pharmaceutical grade or purpose built units are designed specifically for vaccine storage. They feature electronic thermostats, digital displays, alarms and interior fans for uniform air flow. El NSF/ANSI 456 standard sets performance criteria for temperature uniformity, stability and recovery. When purchasing equipment:
Verify that units meet NSF/ANSI 456 certification and ask manufacturers for proof.
Ensure units can maintain 2 °C–8 °C or –50 °C– –15 °C consistently and recover quickly after the door opens.
Choose units with enough space for your largest expected inventory and allow room for air circulation.
Household units and what to avoid
If a pharmaceutical grade unit is unavailable, a stand alone household refrigerator or freezer may be used temporarily. Sin embargo, combination refrigerator/freezers should not be used for vaccine storage because they cannot keep both compartments at safe temperatures. Dormitory style units with a single exterior door pose a significant risk of freezing and are unacceptable.
Avoid placing vaccines in vegetable bins or door shelves—these areas experience the greatest temperature fluctuations. Never store vaccines alongside food or employee lunches; repeated door openings disturb temperature stability.
Placement and auxiliary equipment
Proper placement and accessories help maintain stable temperatures:
Central placement: Store vaccines in the middle of shelves, away from walls, floor and vents.
Thermal ballast: Use non frozen water bottles in refrigerators and frozen water bottles in freezers to stabilize temperatures and support emergency transport.
Data logger probe location: Affix the DDL probe near the vaccines, not on the wall or door.
Power management and emergency preparedness
Power continuity is essential for vaccine cold chain standards. Siga estas pautas:
Do not unplug vaccine storage units or use power strips, surge protectors or extension cords. Plug units directly into wall outlets, ideally on dedicated circuits.
Post “DO NOT UNPLUG” signs at outlets and circuit breakers.
Have a backup refrigerator or freezer and keep it ready in case of primary unit failure. Document its ability to maintain required temperatures.
Prepare an emergency transport kit with conditioned water bottles, coolant packs, labels and separate containers for refrigerated and frozen vaccines..
Consider a generator or uninterruptible power supply capable of maintaining cold storage for at least 72 horas. During an outage, monitor temperatures closely. If they approach the upper or lower limits, transfer vaccines to the backup unit or alternate facility promptly.
Practical equipment tips
Set thermostats mid range (≈ 5 °C for refrigerators, –25 °C for freezers) to buffer minor fluctuations.
Rotar material using a first expired, first out system.
Label areas clearly for refrigerated vs. frozen vaccines; do not store diluents or unrelated materials.
Use water bottles to fill empty space; this helps maintain stable temperatures.
ejemplo real: After a storm knocked out power, staff implemented their contingency plan and moved vaccines to a backup unit with documentation showing it maintained 2 °C-8 °C. Because they had separate packing containers and conditioned water bottles ready, the transfer was smooth and no doses were wasted.
How should you monitor and handle vaccine cold chain emergencies?
Continuous monitoring and rapid response are the heart of cold chain management. Digital data loggers not only track temperature but also alert staff to deviations so corrective action can be taken promptly.
Registradores de datos digitales: features and benefits
A registrador de datos digitales (DDL) is a device that records temperatures at regular intervals and displays current, minimum and maximum readings. The CDC recommends DDLs with the following features:
| Característica | Por que importa | Benefit to your facility |
| Buffered probe | Measures the liquid temperature rather than air, reflecting true vaccine temperature | Prevents false alarms when doors open; protects vaccines from unnecessary transfers |
| Out of range alarm | Alerts staff immediately when temperatures deviate from the safe range | Enables rapid corrective action to save vaccines |
| Programmable logging interval | Allows temperature recording at least every 30 minutos | Provides detailed trend data to analyze fluctuations and comply with regulations |
| Calibration certificate | Confirms device accuracy with uncertainty ±0.5 °C | Ensures audit readiness and supports quality assurance |
| Downloadable data & conectividad | Provides remote access and long term analysis | Enables predictive maintenance and easier reporting |
Use backup DDLs to monitor vaccines during transport or while the primary logger is being replaced. Place the probe near the vaccines and check that calibration certificates are current. If the device fails, call your vaccine program for immediate replacement.
Temperature monitoring procedures
Check and document min/max temperatures twice daily—at the start and end of each workday.
Review logs for completeness and out of range temperatures at least every two weeks and after any excursion. Keep records for at least three years.
If temperatures deviate, label affected vaccines “Do NOT Use,” separate them from other stock and document the event (date, tiempo, temperaturas, descripción, inventario).
Contact your immunization program or vaccine manufacturer for guidance and provide DDL data.
Implement your emergency SOPs. Transfer vaccines to a backup unit if necessary; never leave them in a malfunctioning unit.
Developing SOPs and training staff
Written Standard Operating Procedures (Sops) are essential. They should cover routine storage, monitoreo de temperatura, gestión de inventario, emergency response and transport procedures. Update SOPs annually and whenever guidelines or vaccines change. Assign a primary vaccine coordinator and an alternate to oversee ordering, recepción, seguimiento y respuesta a emergencias.
Training is critical:
Provide orientation for new staff who handle vaccines and annual refresher training for all staff involved in immunization.
Conduct scenario based emergency drills quarterly to assess readiness for fires, power outages or natural disasters.
Highlight common errors such as storing vaccines in vegetable bins or combining them with food.
Ensure every staff member knows where SOPs are kept and how to access emergency contacts.
A good SOP also includes a transport plan: contact your vaccine program before transporting vaccines, prepare separate containers for refrigerated and frozen vaccines, and always use a data logger during transport.
Practical tips for emergency response
Label and quarantine suspected compromised vaccines until guidance is received.
Keep an updated list of manufacturer contact numbers in your SOP.
Check basics first—power supply, unit doors, thermostat settings—and do not silence alarms until the cause is identified.
Use backup power or transport vaccines to a pre arranged backup facility when an outage is prolonged.
Escenario práctico: A clinic discovered a DDL alarm at 6 AM. Staff checked the min/max temperatures (34 °F y 39 °F) and found the refrigerator door slightly ajar. Because they followed SOPs and recorded temperatures, vaccines remained within range and were not wasted.
How to develop accountability and coordination
Assigning roles improves accountability and prevents gaps in cold chain management. A primary vaccine coordinator y alternate should oversee ordering, recepción, monitoreo de temperatura, stock rotation and emergency response. Rotating stock ensures short dated vaccines are used first, while marking public and private inventory helps separate budgets. Regularly update contact lists and designations—especially if coordinators take extended leave.
Latest developments and trends in vaccine cold chain management (2025)
Descripción general de la tendencia
Technological innovation and regulatory updates are reshaping vaccine cold chain standards in 2025:
Expansión del mercado: The market for vaccine shippers is projected to grow from US$1.5 billion in 2024 to US$3.5 billion by 2033.
Adoption of NSF/ANSI 456: This standard sets baseline requirements for vaccine refrigerators and freezers, ensuring temperature uniformity, stability and rapid recovery. Facilities are increasingly seeking certified units and demanding proof of compliance.
Monitoreo digital: IoT enabled DDLs with cloud connectivity allow remote temperature monitoring and predictive maintenance. Some devices can send SMS or app alerts when temperatures deviate, improving response times.
Solar powered and low energy units: In areas with unreliable electricity, solar refrigerators and phase change materials are being deployed. ellos mantienen 2 °C–8 °C without continuous power, enhancing vaccine access.
Data analytics and AI: Advanced analytics help predict equipment failures and optimize inventory management, reduciendo el desperdicio.
Último progreso de un vistazo
Wireless DDLs: Provide real time data to centralized dashboards, enabling regional coordinators to track multiple facilities simultaneously.
Standardized training programs: Online modules and virtual reality simulations improve staff competency and retention of cold chain procedures.
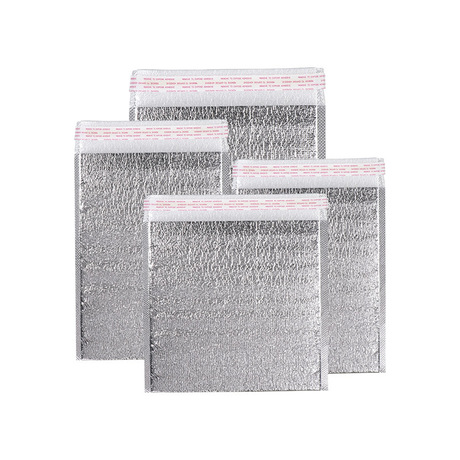
Enhanced packaging: Eco friendly, reusable insulated containers with phase change gel packs maintain temperatures longer, Reducción del impacto ambiental.
Policy updates: Many jurisdictions now mandate documented emergency drills and backup power sources as part of licensing.
Ideas del mercado
Demand for cold chain solutions is driven by expanded immunization schedules (p.ej., RSV and dengue vaccines) and the increasing use of temperature sensitive biologics. Facilities are investing in purpose built units and remote monitoring to meet regulatory requirements and protect high value inventories. As new vaccines enter the market, expect further refinement of temperature standards and training programs.
Preguntas frecuentes
Pregunta 1: What temperature should vaccines be stored at?
Most routine vaccines require refrigerated storage between 2 °C y 8 °C. Live attenuated and certain COVID 19 vaccines require frozen storage between –50 °C and –15 °C, while mRNA vaccines need ultra cold storage between –90 °C y –60 °C. Always check the manufacturer’s instructions.
Pregunta 2: Can I use a household refrigerator to store vaccines?
A stand alone household refrigerator or freezer may be used temporarily, but combination or dormitory style units are not recommended. For long term storage, choose a pharmaceutical grade unit that meets NSF/ANSI 456.
Pregunta 3: How often should I check vaccine storage temperatures?
Record minimum and maximum temperatures twice daily and review logs regularly. DDLs that record at least every 30 minutes provide detailed data.
Pregunta 4: What should I do during a power outage?
Implement your emergency plan: move vaccines to a backup unit powered by a generator, use conditioned water bottles and separate containers for refrigerated and frozen vaccines. Always keep a data logger with the vaccines.
Pregunta 5: Who is responsible for managing the vaccine cold chain?
Designate a primary vaccine coordinator y alternate to oversee ordering, recepción, escucha, stock rotation, SOP maintenance and emergency response. All staff involved in immunization must receive training.
Resumen y recomendaciones
Maintaining vaccine cold chain standards protects vaccine potency, reduces waste and safeguards public health. Las conclusiones clave de esta guía incluyen:
Store vaccines at the correct temperatures—2 °C–8 °C for most vaccines, –50 °C– –15 °C for certain live vaccines and –90 °C– –60 °C for mRNA vaccines.
Use purpose built, pharmaceutical grade equipment that meets NSF/ANSI 456 standards to ensure temperature uniformity and rapid recovery.
Monitor temperatures continuously with calibrated digital data loggers, record min/max readings twice daily and keep records for three years.
Develop SOPs and train staff regularly on storage, escucha, emergency response and transport procedures.
Prepare for emergencies with backup units, power supplies and transport kits, and practice drills quarterly.
Siguiendo estas recomendaciones, you can protect your vaccine inventory, comply with regulatory standards and ensure that patients receive potent, effective vaccines.
Próximos pasos viables
Assess your current equipment: verify that your refrigerators and freezers maintain the required temperature ranges; consider upgrading to NSF/ANSI 456 certified units.
Implement digital data logging: install NIST certified DDLs with buffered probes on each storage unit and set up automated alerts.
Update your SOPs: review and revise procedures to reflect 2025 pautas, including emergency transport and backup power.
Entrena a tu equipo: schedule orientation and annual refresher training; conduct scenario based drills.
Audit your inventory: rotate stock using first expired, primero en salir; remove expired doses promptly and document waste.
Create an emergency kit: stock conditioned water bottles, coolant packs, labels and backup DDLs; ensure the kit is accessible.
Acerca de Tempk
Templ is a cold chain solutions company specializing in insulated packaging, ice packs and temperature controlled containers. With decades of experience in food and pharmaceutical logistics, nosotros design reusable, eco friendly packaging that maintains 2 °C–8 °C or below for extended periods. Our products feature phase change materials and high performance insulation, ensuring consistent temperatures during transit. Recent innovations include IoT enabled containers that monitor internal temperature and location in real time.
Llamado a la acción: For personalized advice on selecting cold chain equipment or improving your vaccine storage protocols, contacto Templ’s experts. We provide free consultations and customized solutions to help you meet vaccine cold chain standards in 2025 y más allá.