Sistema de cadena de frío de vacunas: ¿Cómo funciona? & Por que importa?
El sistema de cadena de frío para vacunas es la base de los programas de vacunación modernos. Es la red de personas., Equipos y procedimientos que mantienen las vacunas dentro de límites de temperatura seguros desde la fabricación hasta la inyección.. Sin un sistema robusto de cadena de frío para vacunas, Las vacunas pierden potencia rápidamente: los estudios muestran que las vacunas expuestas a temperaturas superiores 8 °C puede perder hasta 20 % de su eficacia en tan solo una hora. Esta guía explica cómo funciona el sistema de cadena de frío de las vacunas., los rangos de temperatura recomendados, monitoreando la tecnología y las tendencias emergentes para que pueda proteger cada dosis.

Qué es el sistema de cadena de frío de las vacunas y por qué es importante – incluyendo los elementos clave (personal, equipos y procedimientos).
Rangos de temperatura seguros para las vacunas y sus categorías – refrigerado, Vacunas congeladas y ultrafrías y las consecuencias de las variaciones de temperatura..
Equipos críticos para almacenamiento y transporte. – refrigeradores, congeladores, registradores de datos digitales y contenedores isotérmicos.
Mejores prácticas de seguimiento y procedimientos operativos estándar – cómo utilizar registradores de datos digitales, registrar temperaturas y capacitar al personal..
Métodos de transporte y opciones de embalaje. – paquetes de gel, hielo seco, Logística habilitada con nitrógeno líquido e IoT.
Innovaciones y tendencias del mercado para 2025 – cadena de bloques, almacenamiento con energía solar, Optimización de rutas de IA y crecimiento del mercado global de logística de la cadena de frío de vacunas.
¿Qué es un sistema de cadena de frío para vacunas y por qué es esencial??
Un sistema de cadena de frío de vacunas garantiza que las vacunas permanezcan dentro del rango de temperatura prescrito durante todo su viaje.. Está compuesto por personal capacitado., Equipos especialmente diseñados y procedimientos operativos estándar.. Sin que estos componentes trabajen juntos, las vacunas pueden estar expuestas a calor o frío dañinos, conduciendo a la pérdida de potencia, Dosis desperdiciadas y brotes de enfermedades prevenibles.. De hecho, la investigación sugiere que cuantos 35 % de las vacunas se ven comprometidas debido al mal manejo de la temperatura, lo que resulta en costosas campañas de revacunación y una reducción de la confianza del público.
Por qué el control de la temperatura protege la potencia
Las vacunas son productos biológicos.. El calor puede degradar proteínas y grasas.; La congelación puede provocar cristales de hielo que dañan su estructura.. La mayoría de las vacunas de rutina requieren refrigeración entre 2 °C y 8 °C. Las vacunas vivas atenuadas, como la varicela y algunas formulaciones contra la COVID 19, requieren congelación entre –50 °C y –15 °C., mientras Las vacunas de ARNm a menudo necesitan un almacenamiento ultrafrío entre –90 °C y –60 °C. Exposición a temperaturas anteriores 8 °C durante sólo una hora puede reducir la potencia en 20 %. En cambio, La congelación de vacunas que contienen aluminio provoca aglomeraciones y daños irreversibles.. Por lo tanto, mantener el rango correcto es fundamental para la eficacia..
Elementos clave del sistema de cadena de frío de las vacunas
El Tres elementos clave del sistema de cadena de frío de vacunas son el personal., equipos y procedimientos:
Personal – un manipulador capacitado de vacunas y cadena de frío gestiona el almacenamiento, monitorea las temperaturas y mantiene registros. En cada instalación debe haber un coordinador designado responsable de capacitar al personal., ordenar inventario e implementar planes de emergencia.
Equipo – refrigeradores especialmente diseñados, congeladores, refrigeradores revestidos de hielo (ILR), cajas frias, Los registradores de datos y los vehículos de transporte garantizan que las vacunas permanezcan dentro del alcance.. El equipo puede ser eléctrico. (alimentado por red eléctrica o solar) o no electrico (bolsas de hielo y transportadores de vacunas).
Procedimientos – procedimientos operativos estándar (Sops) describir cómo cargar unidades, organizar las vacunas por fecha de caducidad, registrar temperaturas y responder a excursiones. Sin procedimientos claros, Los equipos y las personas no pueden evitar los daños causados por la temperatura..
Un sólido sistema de cadena de frío de vacunas protege la potencia de las vacunas, reduce el desperdicio y genera confianza pública.
Cómo funciona el sistema de cadena de frío de vacunas en toda la cadena de suministro
El sistema de cadena de frío de la vacuna comienza en la planta de fabricación y continúa a través de las instalaciones de almacenamiento nacionales y locales hasta la clínica.. En cada enlace, Las temperaturas deben mantenerse y documentarse.. Según la Organización Mundial de la Salud, las vacunas viajan desde el fabricante hasta las tiendas primarias, tiendas de distrito y clínicas a través de vehículos refrigerados o aislados, cajas frías y transportadores de vacunas. Estas etapas de transporte utilizan rangos controlados como +2 °C a +8 °C para vacunas refrigeradas y –15 °C a –25 °C para vacunas congeladas. Cada tienda utiliza equipos como cámaras frigoríficas. (WIC), caminar en congeladores (WIF), refrigeradores y congeladores revestidos de hielo para mantener las dosis seguras.
Fabricación – Las vacunas se producen en condiciones estrictas y se enfrían inmediatamente.. Se empaquetan en viales o jeringas y se colocan en contenedores de envío con registradores de datos y refrigerantes.. Los fabricantes deben coordinarse con los proveedores de logística para prepararse para necesidades de temperatura específicas..
Almacenamiento primario y distrital. – Las cámaras frigoríficas y congeladores reciben envíos a granel. El personal controla las temperaturas al menos dos veces al día y garantiza la rotación de existencias utilizando el "primer producto que vence"., método "primero en salir".
Transporte – Furgonetas aisladas, camiones frigoríficos o cajas frías pasivas trasladan las vacunas a instalaciones regionales o locales. Los registradores de datos viajan con los envíos, registrar las temperaturas al menos cada 30 minutos.
Almacenamiento y administración local – Las clínicas utilizan refrigeradores revestidos de hielo o pequeños congeladores para almacenar las vacunas hasta su administración.. Portadores de vacunas mantienen la temperatura correcta durante las jornadas de divulgación. El personal verifica las temperaturas mínimas y máximas cada día laborable y actualiza los registros..
Manteniendo la cadena de frío de principio a fin, El sistema de cadena de frío de la vacuna garantiza que cada dosis proporcione la protección prevista..
Rangos de temperatura seguros y categorías de vacunas
Diferentes vacunas requieren diferentes condiciones de almacenamiento. Conocer el rango de temperatura requerido para cada tipo de vacuna es esencial para el sistema de cadena de frío de las vacunas.. Las siguientes categorías resumen los principales requisitos.:
| Categoría de vacuna | Rango de temperatura | Vacunas de ejemplo | Significado |
| Refrigerado | 2 °C – 8 °C (36 °F – 46 °F) | Influenza, DTaP, VPH, MMR y la mayoría de las vacunas de rutina | El rango más común. Mantener alrededor 5 °C reduce las fluctuaciones. |
| Congelado | –50°C – –15°C (–58 °F – 5 °F) | Varicela, mox (Jynneos) y algunas vacunas COVID 19 | Requerido para vacunas vivas atenuadas; la exposición a temperaturas más cálidas compromete los componentes virales. |
| ultra frio | –90 °C – –60 °C (–130 °F – –76 °F) | Vacunas de ARNm como Pfizer-BioNTech Comirnaty | Necesario para almacenamiento a largo plazo.. Algunos viales se pueden descongelar y almacenar a 2 °C–8 °C durante hasta diez semanas. |
La mayoría de las vacunas que se utilizan hoy en día pertenecen a la categoría refrigerada y nunca deben congelarse.. La congelación de vacunas con adyuvante de aluminio provoca aglomeración y daños irreversibles. En cambio, algunas formulaciones (p.ej., Vacunas de ARNm) pierde potencia rápidamente si se deja descongelar y debe mantenerse en congeladores ultrafríos o trasladarse a un lugar de almacenamiento refrigerado justo antes de su uso..
Consecuencias de las excursiones de temperatura
Incluso breves desviaciones fuera del rango prescrito pueden tener consecuencias graves.. Una exposición de una hora por encima 8 °C puede reducir la eficacia de la vacuna hasta 20 %. Las vacunas congeladas y descongeladas accidentalmente deben desecharse, y las vacunas ultrafrías que se calientan por encima de –60 °C no se pueden devolver al almacenamiento. Porque la potencia no se puede restaurar., El sistema de cadena de frío de vacunas prioriza la prevención mediante un control y seguimiento precisos de la temperatura..
Equipo esencial para el sistema de cadena de frío de vacunas
Los equipos especialmente diseñados son la columna vertebral del sistema de cadena de frío de las vacunas. Los frigoríficos domésticos no son adecuados porque presentan grandes fluctuaciones de temperatura y una refrigeración desigual. Las siguientes categorías de equipos mantienen las vacunas dentro del alcance:
Refrigeradores y congeladores de calidad farmacéutica. – Estas unidades mantienen temperaturas estables dentro del rango recomendado e incluyen características como alarmas, puertas y estantes con cerradura que permiten el flujo de aire. Refrigeradores revestidos de hielo (ILR) almacenar vacunas en +2 °C a +8 °C y tiene un tiempo de retención de 20 horas a 43 °C, lo que significa que mantienen la temperatura durante los cortes de energía. Los congeladores mantienen entre –15 °C y –25 °C y almacenan bolsas de hielo o vacunas que requieren congelación..
Congeladores ultrafríos – Diseñado para vacunas de ARNm, estas unidades mantienen –90 °C a –60 °C. A menudo requieren energía de respaldo y tienen menor capacidad debido al espesor del aislamiento..
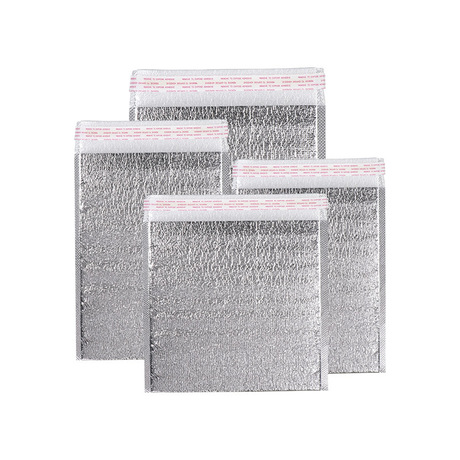
Cajas frías y transportadores de vacunas. – Contenedores pasivos revestidos con aislamiento y llenos de bolsas de hielo condicionadas o materiales de cambio de fase. (PCM). Se utilizan para transporte o sesiones de extensión y pueden mantener +2 °C a +8 °C hasta 96 horas en condiciones de calor.
Furgonetas isotérmicas y vehículos frigoríficos – Vehículos equipados con unidades de refrigeración para el transporte de vacunas entre centros.. Se utilizan tanto para refrigerados (+2 °C a +8 °C) y congelado (–15 °C a –25 °C) productos.
refrigeradores con energía solar – Ideal para áreas remotas sin electricidad confiable. Utilizan paneles solares y baterías para mantener temperaturas de vacunas. El almacenamiento en frío solar reduce los costos de energía; electricidad comercial promediada 13.10 centavos por kilovatio hora en 2024, mientras que las tarifas solares oscilaban entre 3.2 a 15.5 centavos por kWh.
Evitar equipos inadecuados
Se desaconseja el uso de refrigeradores domésticos combinados o refrigeradores estilo dormitorio.. A menudo experimentan fluctuaciones de temperatura y tienen compartimentos congeladores que pueden congelar accidentalmente las vacunas.. Cuando las unidades de grado farmacéutico no están disponibles, Se puede utilizar un refrigerador independiente temporalmente, pero requiere una supervisión cuidadosa.. Coloque siempre las vacunas en sus cajas originales, lejos de paredes y puertas., y nunca almacene alimentos o bebidas en la misma unidad.
Monitoreo de temperatura: Registradores de datos digitales y mejores prácticas
El monitoreo continuo de la temperatura es el corazón del sistema de cadena de frío de las vacunas.. Los EE. UU.. Centros para el Control y la Prevención de Enfermedades (Centros para el Control y la Prevención de Enfermedades) recomienda el uso de registradores de datos digitales (DDL), que registran temperaturas a intervalos preestablecidos y proporcionan historiales detallados. A diferencia de los termómetros simples, Los DDL capturan tendencias y alertan al personal antes de que las vacunas se vean comprometidas.
Características de un registrador de datos digital eficaz
Un DDL confiable debe incluir:
| Característica | Por que importa | Beneficio |
| Sonda tamponada | Mide la temperatura del líquido en lugar del aire., imitando las condiciones de la vacuna | Evita falsas alarmas cuando se abren puertas y reduce traslados innecesarios |
| Alarma fuera de rango | Alerta al personal inmediatamente cuando las temperaturas se desvían | Permite una acción correctiva rápida, Guardar vacunas |
| Intervalo de registro programable | Permite grabar al menos cada 30 minutos | Proporciona un historial de temperatura detallado para auditorías. |
| Calibración y precisión | La incertidumbre de ±0,5 °C y la calibración periódica garantizan lecturas confiables | Garantiza el cumplimiento y protege la potencia de la vacuna. |
| Conectividad en la nube y acceso remoto | Envía datos y alertas en tiempo real a dispositivos remotos | Mejora la supervisión y facilita una respuesta rápida |
Los CDC recomiendan que cada unidad de almacenamiento y transporte tenga un DDL y que al menos un dispositivo de respaldo esté disponible. El personal debe descargar y revisar los datos de DDL al menos cada dos semanas y mantener registros durante tres años.. Los certificados de calibración deben indicar el modelo., número de serie, fecha de calibración, e incertidumbre.
Procedimientos operativos estándar y capacitación
El seguimiento por sí solo es insuficiente sin procedimientos claros y personal capacitado. Cada instalación debe desarrollar procedimientos operativos estándar que cubran el almacenamiento., manejo, escucha, respuesta de emergencia y documentación. Las prácticas clave incluyen:
Registro de temperaturas mínimas y máximas al inicio de cada jornada laboral; si los DDL muestran lecturas mínimas/máximas, el personal todavía los registra diariamente.
Capacitar a todo el personal. quienes manejan las vacunas, con orientación y cursos anuales de actualización. Simulacros basados en escenarios preparan a los equipos para cortes de energía, fallas de equipos y desastres naturales.
Creando un plan de emergencia describir las fuentes de energía de respaldo, ubicaciones de almacenamiento alternativas e información de contacto.
Retención de documentos – mantener registros de temperatura y certificados de calibración durante al menos tres años.
Un SOP sólido garantiza que el sistema de cadena de frío de las vacunas funcione sin problemas incluso durante eventos inesperados..
Transporte y Embalaje: Proteger las vacunas en movimiento
Mantener la temperatura durante el transporte es tan importante como durante el almacenamiento. El sistema de cadena de frío de vacunas utiliza varios métodos de envasado y refrigerantes según el rango de temperatura requerido.. Según una investigación de mercado, El mercado mundial de logística de la cadena de frío de vacunas se valoró en Dólar estadounidense 3.5 mil millones en 2024 y se prevé que alcance los USD 5.9 mil millones por 2034 con una CAGR de 5.3 %. El crecimiento está impulsado por una mayor producción de vacunas, Avances en tecnologías de embalaje y creciente conciencia sobre la salud y el bienestar..
Métodos de embalaje y refrigerantes
hielo seco (dióxido de carbono sólido) – proporciona temperaturas de alrededor de –78 °C y es adecuado para envíos congelados o ultrafríos. Sublima en lugar de derretirse., pero las regulaciones de envío limitan la cantidad que se puede utilizar.
Paquetes de gel y materiales de cambio de fase. (PCM) - mantener 2 °C–8 °C para vacunas refrigeradas. Los PCM absorben o liberan calor a temperaturas específicas, ampliando los tiempos de espera.
Nitrógeno líquido – permite condiciones criogénicas por debajo de –150 °C para terapias celulares y genéticas.
Utilice contenedores validados y empaquete diseños que coincidan con las condiciones ambientales y el tiempo de tránsito esperados.. Incluya siempre un DDL calibrado dentro de los envíos y seleccione rutas de envío que minimicen el tiempo de tránsito y la manipulación..
Sensores habilitados para IoT y logística impulsada por IA
La logística moderna de la cadena de frío depende cada vez más de Sensores inteligentes que transmiten la temperatura en tiempo real., datos de humedad y ubicación. Cuando los sensores detectan temperaturas inseguras, alertan automáticamente a los usuarios a través de mensajes de texto, correo electrónico o aplicación móvil. La integración de sensores con GPS proporciona visibilidad en toda la cadena de suministro y permite una intervención rápida.. Inteligencia artificial (AI) Los algoritmos analizan el tráfico y los datos meteorológicos para optimizar las rutas. y reducir el tiempo de tránsito. El análisis predictivo identifica patrones y activa alertas antes de que se produzcan excursiones, hacer que el sistema de cadena de frío de las vacunas sea más resiliente.
Innovaciones que dan forma al sistema de cadena de frío de las vacunas en 2025
El sistema de cadena de frío de las vacunas está evolucionando rápidamente. Tecnologías emergentes en 2025 mejorar la transparencia, sostenibilidad y eficiencia, ayudar a satisfacer la creciente demanda de vacunas y cumplir con regulaciones más estrictas. destaca varias innovaciones clave:
Blockchain para una trazabilidad de extremo a extremo – La tecnología de contabilidad distribuida registra cada transacción en la cadena de suministro, crear un registro de temperatura a prueba de manipulaciones, eventos de ubicación y entrega. Esta transparencia facilita las auditorías y reduce el riesgo de manipulación de datos..
Almacenamiento en frío con energía solar – Las unidades solares aisladas proporcionan refrigeración confiable en áreas con electricidad inestable. El almacenamiento en frío solar reduce los costos operativos; en 2024 electricidad comercial promediada 13.10 ¢/kWh, mientras que las tarifas solares oscilaban entre 3.2 a 15.5 ¢/kWh.
Sensores inteligentes habilitados para IoT – Los sensores inalámbricos entregan datos y alertas en tiempo real, reducir el riesgo operativo. Junto con GPS, permiten una visibilidad completa desde el origen hasta el destino.
Optimización de rutas impulsada por IA – La IA analiza el tráfico y los patrones climáticos para elegir rutas que mantengan la estabilidad de la temperatura y reduzcan el tiempo de tránsito..
Congeladores criogénicos portátiles – Las unidades compactas mantienen entre –80 °C y –150 °C, Permitir el transporte seguro de terapias celulares y genéticas y vacunas ultrafrías..
Embalaje sostenible – Contenedores reciclables, Las envolturas térmicas biodegradables y las compresas frías reutilizables reducen el impacto ambiental mientras mantienen la temperatura..
Estas innovaciones no sólo mejoran el rendimiento sino que también alinean el sistema de cadena de frío de vacunas con el medio ambiente corporativo., sociales y gobernanza (ESG) compromisos.
Perspectivas del mercado e impulsores del crecimiento
El sector de la cadena de frío apoya tanto a la industria alimentaria como a la farmacéutica, pero las vacunas representan un segmento de alto riesgo. Se espera que el mercado mundial de la cadena de frío crezca desde USD 418.81 mil millones en 2025 a USD 1,416.67 mil millones por 2034, representando un 14.5 % tasa de crecimiento anual compuesta (Tocón). América del Norte tiene aproximadamente 36 % de ingresos y continúa invirtiendo en tecnologías energéticamente eficientes. Al mismo tiempo, El mercado de logística de la cadena de frío dedicada a las vacunas se expandirá desde Dólar estadounidense 3.5 mil millones en 2024 a USD 5.9 mil millones por 2034.
Los impulsores del crecimiento incluyen:
Creciente producción de vacunas – El despliegue en curso de refuerzos de ARNm y terapias celulares requiere una mayor capacidad de la cadena de frío.
Innovaciones tecnológicas – Sensores de IoT, blockchain y la IA mejoran la eficiencia y reducen el desperdicio.
Ampliar el acceso a la atención médica – Los programas de inmunización rural y las iniciativas globales de erradicación de enfermedades requieren almacenamiento en frío confiable en áreas remotas.
Cumplimiento regulatorio – Directrices más estrictas para el control de la temperatura., La documentación y la seguridad obligan a las instalaciones a actualizar los equipos y sistemas..
Enfoque de sostenibilidad – Gobiernos y empresas priorizan la energía renovable y los materiales reciclables en las operaciones de la cadena de frío..
Comprender estas tendencias ayuda a las organizaciones a anticipar las necesidades futuras y planificar las inversiones en consecuencia..
2025 Últimos desarrollos y tendencias
2025 trae nuevos desarrollos que remodelan el sistema de cadena de frío de las vacunas:
Las cadenas de frío conectadas se convierten en la norma – Integración de sensores IoT, La IA y la cadena de bloques fomentan la visibilidad de extremo a extremo y la intervención proactiva. Las instalaciones pueden monitorear los envíos en tiempo real y responder rápidamente a las excursiones..
Cumplimiento y auditoría más estrictos – Organismos reguladores como los CDC, La OMS y el PIB de la UE requieren un seguimiento continuo de la temperatura, mantenimiento de registros detallados y calibración periódica.
Creciente demanda de almacenamiento ultrafrío – La popularidad de los refuerzos de ARNm y los productos biológicos impulsa la inversión en congeladores criogénicos y envases especializados..
Integración de la sostenibilidad – Las empresas adoptan unidades alimentadas por energía solar y envases reciclables para reducir el consumo de energía y los residuos..
Cadena de suministro de vacunas digitales (DVSC) – La tecnología de la información moderna rastrea y gestiona los procesos de vacunación en tiempo real., mejorar la transparencia y la eficiencia. La estrategia global de la Organización Mundial de la Salud sobre salud digital (2020–2025) alienta a los países a aprovechar las tecnologías digitales para mejorar la gestión de la cadena de suministro de vacunas.
Al adoptar estas tendencias, Las organizaciones pueden preparar sus sistemas de cadena de frío para vacunas en el futuro..
Preguntas frecuentes
Q1: ¿Cuánto tiempo se pueden almacenar las vacunas de ARNm a temperatura de refrigerador??
Después de descongelar, Algunas vacunas de ARNm, como Pfizer-BioNTech Comirnaty, pueden mantenerse en 2 °C–8 °C durante hasta diez semanas. Consulte siempre el prospecto del producto del fabricante y controle las temperaturas continuamente..
Q2: ¿Qué debo hacer si una vacuna se expone a temperaturas superiores 8 °C?
Cualquier variación de temperatura puede degradar la potencia.. Inmediatamente poner en cuarentena las vacunas afectadas, Etiquételos como “no usar,” y comuníquese con el fabricante o el programa de vacunación para obtener orientación.. Los estudios demuestran que una exposición de una hora por encima 8 °C mayo reducir la eficacia de la vacuna hasta 20 %. Nunca administrar dosis comprometidas.
Q3: ¿Puedo usar un refrigerador doméstico para almacenar vacunas??
Los refrigeradores domésticos sólo se pueden utilizar si no hay unidades de calidad farmacéutica disponibles.. No se aceptan unidades combinadas ni refrigeradores estilo dormitorio.; tienen temperaturas desiguales y pueden congelar las vacunas. Si se utiliza un refrigerador doméstico, colocar vacunas en el centro, lejos de las paredes y la puerta, y controlar las temperaturas de cerca.
Q4: ¿Con qué frecuencia debo registrar las temperaturas??
Los CDC recomiendan verificar y documentar las temperaturas mínimas y máximas. al menos dos veces al día y descargar datos de registradores digitales cada dos semanas o después de cualquier excursión. Si su registrador muestra lecturas mínimas/máximas, registrarlos al inicio de cada jornada laboral.
Q5: ¿Qué debe incluir un plan de emergencia para la cadena de frío??
Un plan sólido debe cubrir fuentes de energía de respaldo, ubicaciones de almacenamiento alternativas, contenedores de transporte e información de contacto de emergencia. Realice simulacros periódicos y asegúrese de que todo el personal conozca los pasos para transferir las vacunas de manera segura durante cortes de energía o fallas en el equipo..
Resumen y recomendaciones
En 2025 El sistema de cadena de frío de las vacunas es más crítico que nunca.. Mantener la potencia de las vacunas requiere un estricto cumplimiento de los rangos de temperatura (2 °C–8 °C para la mayoría de las vacunas, –50 °C– –15 °C para vacunas vivas atenuadas y –90 °C– –60 °C para formulaciones de ARNm). Utilice refrigeradores de calidad farmacéutica., congeladores y unidades de ultra frío; Evite los refrigeradores combinados del hogar y el hacinamiento.. Implementar registradores de datos digitales calibrados con sondas tamponadas, alarmas y conectividad en la nube para monitorear las temperaturas continuamente. Desarrollar procedimientos operativos estándar, capacitar al personal regularmente, y prepararse para emergencias. Abarcar innovaciones como sensores de IoT, Optimización de rutas de IA, Trazabilidad blockchain y almacenamiento con energía solar. para mejorar la eficiencia y la sostenibilidad. Finalmente, manténgase informado sobre tendencias del mercado, cambios regulatorios y nuevas tecnologías para preparar su sistema de cadena de frío de vacunas para el futuro.
Plan de acción: Próximos pasos para optimizar su sistema de cadena de frío de vacunas
Audita tu equipo – Evalúa tus frigoríficos actuales, congeladores y registradores de datos. Reemplace cualquier combinación o unidades estilo dormitorio con modelos de grado farmacéutico. Verificar los certificados de calibración y planificar reemplazos para unidades que se acercan al final de su vida útil..
Implementar o actualizar el monitoreo digital – Invertir en registradores de datos digitales de alta precisión con sondas tamponadas con glicol, alarmas fuera de alcance y conectividad en la nube. Asegúrese de que el intervalo de registro sea al menos cada 30 minutos y mantener dispositivos de respaldo.
Desarrollar SOP integrales y programas de capacitación. – Crear procedimientos escritos que cubran el almacenamiento., transporte, seguimiento y respuesta a emergencias. Capacitar a todo el personal al momento de la contratación y brindar cursos de actualización anuales.. Realizar simulacros periódicos para probar el plan de emergencia..
Explora las innovaciones y la sostenibilidad – Evaluar la viabilidad de refrigeradores con energía solar para sitios fuera de la red y sensores de iot para monitoreo en tiempo real. Considere opciones de embalaje sostenibles, como contenedores reutilizables y envoltorios térmicos biodegradables..
Monitorear las actualizaciones regulatorias y del mercado. – Manténgase informado sobre la evolución de las pautas de los CDC, OMS y autoridades nacionales. Monitorear las tendencias del mercado, como el crecimiento del mercado de logística de la cadena de frío de vacunas y las tecnologías emergentes..
Siguiendo este plan de acción podrás fortalecer tu sistema de cadena de frío de vacunas, reducir el desperdicio y garantizar que cada dosis administrada proporcione inmunidad total.
Acerca de Tempk
Tempk es un innovador líder en soluciones de cadena de frío para la atención médica y las ciencias biológicas.. Diseñamos y fabricamos refrigeradores de grado farmacéutico., congeladores, contenedores aislados y sistemas de control de temperatura de última generación. Nuestros productos cuentan con aislamiento avanzado., registradores de datos digitales con conectividad a la nube y opciones para integración de energía solar, permitiendo un almacenamiento confiable en ubicaciones remotas. Estamos comprometidos con la sostenibilidad y ofrecemos envases reutilizables y envoltorios térmicos biodegradables para reducir el impacto ambiental.. Con una R dedicada&Equipo D y estrictos estándares de calidad., nosotros te ayudamos salvaguardar las vacunas y apoyar el cumplimiento normativo.
Listo para optimizar su sistema de cadena de frío de vacunas? Contacta con nuestros especialistas hoy para una evaluación personalizada y descubra cómo Tempk puede ayudarle a mantener la potencia, reducir el desperdicio y adoptar las innovaciones de 2025.