Maintaining vaccine potency depends on cold chain vaccine storage and handling. In 2025, Impfprogramme werden weiter ausgeweitet, and the market for vaccine shippers alone is projected to grow from USD 1.5 Milliarden in 2024 in USD 3.5 Milliarden von 2033. Doch eine Temperaturabweichung außerhalb des zulässigen Bereichs kann ein Fläschchen zerstören. Die meisten Impfstoffe erfordern gekühlte Temperaturen dazwischen 2 °C und 8 °C, some freeze below –15 °C and a few mRNA formulations need ultra cold storage as low as –90 °C. Richtige Handhabung, Überwachung und Notfallplanung sind unerlässlich. Dieser Leitfaden entmystifiziert den Prozess, Konzentration auf die Ausrüstung, Verfahren und Innovationen, die die Sicherheit von Impfstoffen gewährleisten.
Temperaturbereiche: Welche Temperaturbereiche werden für die Lagerung von Impfstoffen empfohlen?, und warum ist ein enger Bereich kritisch??
Ausrüstungsauswahl: Wie wählt man Kühlschränke aus?, Gefriergeräte und Ultrakühlgeräte, die für verschiedene Impfstofftypen geeignet sind?
Überwachung & Sops: Welche Geräte und Verfahren sorgen dafür, dass die Temperaturen im zulässigen Bereich bleiben?, und wie sollten Sie reagieren, wenn dies nicht der Fall ist??
Ausbildung & Koordinierung: Wer ist für das Kühlkettenmanagement verantwortlich?, and what training and standard operating procedures (Sops) sind erforderlich?
Aufkommende Trends: What innovations, market dynamics and regulatory changes in 2025 influence vaccine cold chain management?
Practical Tips & FAQs: How can you apply best practices, avoid pitfalls and protect your inventory during an emergency?
What Are the Recommended Temperature Ranges and Why Do They Matter?
Vaccines are biological products that lose potency outside their prescribed temperature ranges. Standard refrigerators must maintain 2 °C–8 °C (36 °F–46 °F). Frozen vaccines like varicella and some COVID 19 formulations require –50 °C bis –15 °C (–58 °F bis 5 ° F), while ultra cold mRNA vaccines are stored between –90 °C und –60 °C (–130 °F bis –76 °F). Exposure above or below these ranges can degrade proteins, destabilize lipids and render the vaccine ineffective. Overheating is like leaving a cake out in the sun—essential ingredients break down; freezing certain vaccines forms ice crystals that damage molecular structures.
Maintaining these ranges is not optional. The CDC recommends recording minimum and maximum temperatures at least twice daily and using calibrated digital data loggers (DDLs) um die Temperaturen kontinuierlich zu verfolgen. In 2025, some vaccine vials (such as mRNA COVID 19 vaccines) can be transferred from ultra cold to refrigerated conditions for limited periods; Zum Beispiel, the Pfizer BioNTech Comirnaty vaccine may be stored between 2 °C und 8 °C für bis zu 10 Wochen nach dem Auftauen. Adhering to these guidelines prevents costly revaccination and protects public trust.
Choosing Appropriate Storage Equipment
Selecting the right storage unit depends on the vaccine’s temperature requirements and facility capacity. Zweckmäßig gebaut, pharmaceutical grade refrigerators and freezers are preferred; if unavailable, stand alone household units can be used, but combination refrigerator/freezers are not recommended. Dorm style units with a single exterior door should never be used because they pose a significant risk of freezing vaccines. Each storage unit should have enough space to hold the largest expected inventory (Z.B., during flu season) without crowding.
| Gerätetyp | Empfohlener Temperaturbereich | Impfstoffe gelagert | Praktische Bedeutung |
| Pharmaceutical Grade Refrigerator | 2 °C–8 °C (36 °F–46 °F) | Grippe, DTaP, HPV, MMR und die meisten Routineimpfungen | Stable temperatures protect potency; a stand alone unit prevents freezing from a shared freezer compartment |
| Medical Freezer | –50 °C– –15 °C (–58 °F–5 °F) | Varizellen, mpox (Jynneos) and some COVID 19 vaccines like Moderna Spikevax | Separate freezer prevents warm air from circulating onto refrigerated vaccines; manual defrost units require regular maintenance |
| Ultrakalter Gefrierschrank | –90 °C– –60 °C (–130 °F– –76 °F) | mRNA-Impfstoffe (Z.B., Pfizer BioNTech Comirnaty), fortschrittliche Biologika | Specialized units with alarms and backup power; vital for high value biologics |
Praktische Tipps und Ratschläge
Use purpose built units: Choose pharmaceutical grade refrigerators and freezers; avoid dormitory or “bar” units that risk freezing vaccines.
Stellen Sie die Thermostate auf den mittleren Bereich ein: Adjust to approximately 5 °C for refrigerators and –25 °C for freezers to minimize fluctuations
Organize inventory: Keep vaccines in their original boxes to protect from light and track expiry dates; arrange by type and expiration to practice first expired, zuerst raus (FEFO).
Vermeiden Sie Überfüllung: Allow space for air circulation by storing vaccines in the center of shelves and using water bottles to help stabilize temperature.
Beschriften Sie es deutlich: Legen Sie Regale für gekühlte und gefrorene Impfstoffe fest; Lagern Sie keine Verdünnungsmittel oder Lebensmittel in Impfeinheiten.
Beispiel aus der realen Welt: In 2024 a clinic in upstate New York avoided wasting über USD 20,000 worth of vaccines when a freezer failed. Staff had a backup unit, maintained documentation showing the backup could maintain 2 °C–8 °C, and executed their emergency plan to transfer the inventory quickly.
How Should You Monitor and Manage Vaccine Cold Chains?
Continuous monitoring and clear procedures are the heart of vaccine cold chain management. The CDC requires each storage unit to be equipped with a digitaler Datenlogger (DDL) das mindestens alle Temperaturen aufzeichnet 30 Minuten. A DDL must have a buffered temperature probe, Alarm außerhalb des zulässigen Bereichs, low battery indicator, display of current, minimum and maximum temperatures, and an uncertainty of ±0.5 °C. Facilities should also maintain backup DDLs and ensure calibration certificates are current.
Temperature data should be reviewed and downloaded at least every two weeks and whenever an excursion occurs. Documentation should be kept for at least three years to comply with audit requirements. Staff must check and record min/max temperatures at the start of each workday. If a device doesn’t display min/max readings, temperatures must be checked at least twice daily. Regular calibration ensures accuracy.
Developing Standard Operating Procedures and Training Staff
Every facility should create and maintain written Standardarbeitsanweisungen (Sops) deckt routinemäßige Lagerung und Handhabung ab, emergency procedures and general information. SOPs should be updated annually by the vaccine coordinator and reviewed by staff. Schulung ist entscheidend: all staff who handle vaccines must receive orientation and annual refresher training; additional training is required when new vaccines are introduced or guidelines change.
A designated Impfkoordinator and alternate oversee ordering, receiving and monitoring vaccines; they ensure temperature logs are recorded, Lager drehen, respond to excursions and manage transport. Good procedures emphasise verifying packaging upon delivery, checking temperature indicators and reporting discrepancies.
| DDL-Funktion | Warum ist es wichtig | Benefit to Your Facility |
| Gepufferte Sonde | Misst die Flüssigkeitstemperatur statt der Luft, spiegelt die tatsächliche Impfstofftemperatur wider | Verhindert Fehlalarme beim Öffnen von Türen; schützt Impfstoffe vor unnötigen Übertragungen |
| Alarm bei außerhalb des zulässigen Bereichs liegenden Temperaturen | Warnt das Personal sofort, wenn die Temperaturen vom sicheren Bereich abweichen | Ermöglicht schnelle Korrekturmaßnahmen zur Einsparung von Impfstoffen |
| Programmierbares Protokollierungsintervall | Ermöglicht die Temperaturaufzeichnung mindestens alle 30 Minuten | Provides detailed trend data to analyse fluctuations and comply with regulations |
| Kalibrierzertifikat | Bestätigt die Gerätegenauigkeit mit einer Unsicherheit von ±0,5 °C | Stellt die Auditbereitschaft sicher und unterstützt die Qualitätssicherung |
| Herunterladbare Daten & Konnektivität | Bietet Fernzugriff und Langzeitanalyse | Ermöglicht vorausschauende Wartung und einfachere Berichterstellung |
Notfallvorsorge: Responding to Excursions
Trotz aller Bemühungen, equipment failures or power outages can happen. The CDC advises facilities to have contingency plans that include backup power (Z.B., generators capable of maintaining cold storage for 72 Std.) and an alternative storage facility within the required temperature range. Transport plans should outline how to pack vaccines with conditioned water bottles or cold packs and separate refrigerated and frozen vaccines. Maintain a contact list for building management, security and health departments. Vaccines exposed to questionable temperatures should be labeled “Do NOT Use” until viability is confirmed.
Praktisches Szenario: Eine öffentliche Apotheke bemerkte einen DDL-Alarm 6 BIN. Das Personal zeichnete die Mindest-/Höchsttemperaturen auf (34 °F und 39 ° F) and discovered that the refrigerator door was slightly ajar overnight. Denn sie haben die Temperaturen dokumentiert und zeitnah reagiert, Die Impfstoffe blieben in Reichweite und wurden nicht verschwendet.
Who Is Responsible for Cold Chain Management?
Accountability is vital for protecting vaccines. A primary vaccine coordinator and an alternate must be appointed to ensure proper storage and handling. Coordinators are responsible for ordering vaccines, organising and rotating stock, setting up temperature monitoring devices and responding to excursions. They must also develop and update SOPs, train staff and oversee emergency preparations.
Facilities must provide regular training so that all staff understand procedures and know where to find SOPs. Training should occur during new employee orientation, annually for all staff involved in immunisation activities and whenever new vaccines or updated recommendations are introduced. This ensures that everyone knows how to read DDL alarms, record temperatures and implement contingency plans.
Internal Audits and Continuous Improvement
Periodic internal audits help identify gaps and opportunities for improvement. Review temperature logs for trends, check calibration dates, verify that staff documentation is complete and test emergency procedures. Evaluate the performance of storage units, including door seals, temperature stability and alarm functionality. Continuous improvement fosters resilience and reduces waste.
What Innovations and Trends Are Shaping Vaccine Cold Chain Management in 2025?
Rapid technological advances and market dynamics are transforming vaccine cold chains. The vaccine shippers market is forecast to grow at a CAGR von rund 10 %, erhebt sich von USD 1.5 Milliarden in 2024 in USD 3.5 Milliarden von 2033. Demand is fueled by rising vaccine production, new biologics and global immunization programs. Nordamerika hält derzeit 40 % of the vaccine shippers market, with Asia Pacific growing fastest at a 10 % CAGR, reflecting increasing healthcare investment. Passive vaccine shippers dominate with a 60 % Marktanteil, while reusable units are the fastest growing sub segment due to sustainability goals.
Neue Technologien
KI und Predictive Analytics: Modern DDLs and cloud platforms use machine learning to identify patterns in temperature data and predict equipment failures, Ermöglicht eine proaktive Wartung. AI also supports route optimization and real time visibility across the supply chain.
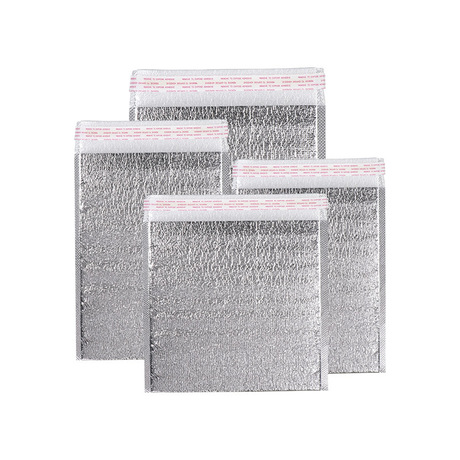
High Performance Insulated Packaging: Passive shippers with advanced phase change materials and vacuum insulation can maintain ultra cold temperatures for 96 hours or longer without dry ice, Reduzierung des CO2-Fußabdrucks. Reusable shippers help reduce waste and lower cost of ownership.
Solar Powered and Off Grid Refrigerators: Solar direct drive fridges and vaccine coolers are increasingly adopted in remote areas to ensure reliable cold storage where electricity is unreliable.
Digital Traceability and Blockchain: Blockchain and connected devices create immutable records of temperature data and chain of custody, enhancing compliance with Good Distribution Practices and fostering trust among stakeholders.
IoT enabled Transport: GPS enabled temperature sensors track shipments in real time, sending alerts when thresholds are exceeded. These systems integrate with logistics platforms to provide a holistic view of the cold chain and facilitate rapid interventions.
Marktwachstum und regionale Trends
| Indikator | Value and Trend | Implikation |
| Marktgröße (Vaccine Shippers) | USD 1.5 B in 2024, projiziert auf USD 3.5 B von 2033 | Signals a growing need for specialised packaging and transport solutions |
| Industry Value | CDC projects the vaccine storage and transportation industry to reach USD 2.4 B von 2025 | Highlights investment in infrastructure and technology |
| Dominant Region | Nordamerika hält 40 % Marktanteil; Europa 30 %; Asien-Pazifik 20 % | Shows developed markets lead but Asia is catching up |
| Am schnellsten wachsende Region | Asien-Pazifik, mit a 10 % CAGR aus 2023 Zu 2028 | Reflects expanding vaccination programs and logistic investments |
| Top Sub Segment | Passive vaccine shippers hold 60 % Marktanteil; reusable units are growing fastest | Indicates sustainability initiatives and cost savings |
Real World Innovation Example
During the initial rollout of mRNA COVID 19 vaccines, limited access to ultra cold freezers led to the development of specialized shipping boxes filled with dry ice. These boxes allowed vaccines requiring –70 °C storage to be transported globally without dedicated freezers, demonstrating how packaging innovation can overcome infrastructure gaps.
2025 Developments and Trends in Vaccine Cold Chain Storage and Handling
In 2025, vaccine cold chain management continues to evolve as new technologies and regulations take hold. Gute Vertriebspraxis (BIP) Richtlinien now require validated equipment, temperature mapping and robust documentation for pharmaceutical logistics. The FDA’s cGMP regulations emphasize proper storage and distribution procedures. These rules underline the need for continuous monitoring and quality assurance throughout the supply chain.
Vaccine programs in low and middle income countries are expanding, creating demand for sustainable off grid refrigeration and cost effective passive shippers. Investment in digital health infrastructure means more facilities integrate cloud connected DDLs and remote management tools. With the growth of personalized medicine and gene therapies, demand for ultra cold storage will likely surge.
Latest Advancements Overview
AI Driven Monitoring: DDLs with predictive analytics forecast potential equipment failures, reducing downtime and vaccine loss.
Reusable Passive Shippers: High performance containers using phase change materials and vacuum insulation provide up to 96 hours of temperature hold time without dry ice.
Intelligente Etiketten & Indicators: Zeit-Temperatur-Indikatoren (TTIs) and NFC tags visually signal temperature excursions, enhancing last mile quality control.
Solar & Battery Backed Refrigeration: Off grid solutions support immunization campaigns in remote areas lacking stable electricity.
Blockchain für Rückverfolgbarkeit: Immutable records of temperature and custody create transparent supply chains and improve regulatory compliance.
Markteinsichten
The vaccine cold chain market benefits from global initiatives such as Gavi’s COVAX program and WHO’s Immunization Agenda 2030, which aim to expand vaccine access and strengthen supply chains. Jedoch, fast 20 million children worldwide missed basic vaccines in 2021, underscoring logistical challenges. As governments invest in cold chain infrastructure, the market for vaccine shippers and monitoring devices will continue to grow, with reusable and sustainable solutions gaining traction.
Häufig gestellte Fragen
Q1: Welchen Temperaturbereich benötigen die meisten Impfstoffe??
Most routine vaccines such as influenza, Masern, mumps, rubella and tetanus should be stored in refrigerators maintained at 2 °C–8 °C (36 °F–46 °F). Live attenuated vaccines like varicella and some COVID 19 products require freezers set between –50 °C und –15 °C, while certain mRNA vaccines need ultra cold storage between –90 °C und –60 °C. Always check the manufacturer’s package insert for specific products.
Q2: How often should I check and record vaccine storage temperatures?
You should check and record minimum and maximum temperatures at the start of every workday. If your device does not display min/max temperatures, Notieren Sie mindestens zweimal täglich die aktuelle Temperatur. Zusätzlich, download data from your digital data logger at least every two weeks or whenever an excursion occurs.
Q3: What equipment do I need to store mRNA vaccines?
mRNA vaccines like Pfizer BioNTech Comirnaty require ultra cold freezers that can maintain –90 °C bis –60 °C. These units must have alarms, backup power and dedicated digital data loggers. If vaccines are moved to refrigeration, follow manufacturer guidelines—Comirnaty can be stored at 2 °C–8 °C für bis zu 10 Wochen nach dem Auftauen.
Q4: Who is responsible for vaccine cold chain management in my facility?
Each facility must designate a primary vaccine coordinator and an alternate who oversee ordering, receiving and storing vaccines, record temperatures, respond to excursions, train staff and maintain SOPs. They must ensure compliance with guidelines and coordinate emergency plans.
Zusammenfassung & Empfehlungen
Maintaining vaccine potency in 2025 demands vigilant cold chain vaccine storage and handling. Key Takeaways:
Follow specific temperature ranges: Keep refrigerated vaccines at 2 °C–8 °C and use separate freezers for –50 °C– –15 °C Impfungen; employ ultra cold units for –90 °C– –60 °C Biologika.
Use proper equipment and monitoring: Choose purpose built units, install DDLs with buffered probes, alarms and calibration certificates and record temperatures at least twice daily.
Develop SOPs and train staff: Create written procedures covering routine and emergency handling, assign vaccine coordinators and provide annual training.
Bereiten Sie sich auf Notfälle vor: Maintain backup power and alternative storage sites, pack vaccines properly for transport and label questionable doses “Do NOT Use”.
Umfassen Sie Innovation: Adopt AI enabled monitoring, reusable passive shippers and solar powered refrigeration to enhance resilience and sustainability.
Nächste Schritte: Audit your facility’s cold chain equipment and protocols. SOPs aktualisieren, verify DDL calibration certificates, schedule staff training and invest in emerging technologies that align with your mission. A proactive approach reduces waste, protects patients and ensures compliance with evolving regulations.
Über Tempk
Tempk delivers integrated cold chain solutions for pharmaceuticals and biologics. Wir offer purpose built refrigerators, Gefrierschränke und Ultrakühlgeräte, high performance insulated shippers and IoT enabled monitoring platforms. Our products are validated to meet Good Distribution Practice requirements and come with calibration certificates for regulatory audits. Wir also provide training and consultancy services to help facilities implement SOPs and emergency plans. By combining sustainable materials with cutting edge technology, Tempk helps healthcare providers safeguard vaccines and reduce environmental impact.
Ready to optimise your vaccine cold chain? Contact us for a personalised assessment and discover how Tempk can help you maintain compliance and protect patient safety.