How to protect vaccines in the cold chain?
Updated in November 2025, this comprehensive guide walks you through everything you need to know about cold chain vaccine storage, from recommended temperature ranges to the latest innovations and market trends. Proper storage keeps vaccines safe and potent, and missteps can result in waste and public health risks. In this article you’ll learn practical strategies, case studies and expert insights that help you preserve vaccine efficacy and comply with regulations.
Why is maintaining the 2°C–8°C range so critical? Discover how temperature excursions quickly degrade vaccine potency and lead to waste.
What equipment and materials do you need for different vaccine types? We detail the differences between refrigerated, frozen and ultra-cold vaccines and the hardware that suits each.
How does cold chain technology evolve in 2025? Découvrez comment l'IA, IoT sensors and sustainable packaging are reshaping vaccine logistics.
What best practices reduce errors and ensure compliance? Learn how inventory management, temperature monitoring and staff training prevent costly mistakes.
Where is the market heading? Get up to date figures on market size, growth rates and regional trends for cold chain monitoring and vaccine storage.
Why is temperature control so critical for vaccines?
Temperature affects vaccine potency: Vaccines and biologics are sensitive molecules; outside their recommended ranges proteins denature and lose effectiveness. Le World Health Organization estimates that nearly half of vaccines are wasted because of inadequate temperature control. Entre-temps, plus que 85 % des produits biologiques nécessitent un stockage réfrigéré, and cell and gene therapies often demand cryogenic temperatures down to −80 °C.
What temperatures apply to different vaccines?
| Storage Category | Recommended Range | Exemples | Pourquoi ça compte pour toi |
| Refrigerated vaccines | 2 ° C - 8 ° C (36 °F – 46 °F) | COVID 19 (Comirnaty, Novavax), DTaP, HepA/B, influenza and most childhood vaccines | A standard medical refrigerator paired with phase change materials and data loggers maintains this range. These vaccines represent the majority of routine immunisations. |
| Vaccins congelés | –50 °C à –15 °C (–58 °F to 5 °F) | Varicella, mpox (Jynneos) and certain combination vaccines | Freezers with precise thermostats and alarms preserve live attenuated vaccines. Their fragility demands consistent sub zero temperatures. |
| Ultra cold vaccines | –90 ° C à –60 ° C (–130 °F to –76 °F) | Some COVID 19 mRNA vaccines (e.g. Pfizer BioNTech Comirnaty) | Ultra cold freezers or portable cryogenic shippers are required; storing outside these ranges can render the vaccine ineffective. |
How do different therapies increase complexity?
Understanding categories helps you select appropriate equipment. Vaccins standards and peptides rely on insulated shippers and gel packs to stay within 2 ° C - 8 ° C. Biologique such as insulin and monoclonal antibodies may be refrigerated short term but need freezers (–20 °C à –80 °C) for long term stability. Thérapies cellulaires et géniques demand cryogenic storage (–80 °C à –150 °C) via specialized freezers or liquid nitrogen vapour, plus validated portable shippers for clinic deliveries. Matching your product portfolio to these categories is the first step toward successful cold chain management.
Best practices for reliable vaccine storage
Invest in proper equipment: Le CDC recommends pharmaceutical grade refrigerators with calibrated thermostats and alarms for vaccine storage. Household refrigerators often lack uniform temperature distribution, and their freezer compartments are unsuitable for vaccines. For frozen vaccines, freezers with precise temperature control and remote monitoring are essential. Use of digital data loggers and continuous monitoring helps detect excursions quickly.
Organize and label effectively: Keep vaccines in their original packaging and store them in the centre of shelves, away from walls, doors and vegetable bins. Use inventory labels to minimize errors and rotate stock based on expiration dates. Overcrowding impedes airflow; leaving space promotes uniform temperatures.
Monitor temperatures diligently: The CDC guidelines urge checking and recording minimum and maximum temperatures at least twice per day. If your devices don’t display min/max readings, record the current temperature at the beginning and end of each workday. Pour les expéditions longues, continuous monitoring with IoT sensors provides real time alerts and audit trails.
Formez votre personnel: Storage errors often stem from human factors. Provide training on loading procedures, temperature logging, recognizing compromised vaccines, et intervention d'urgence. Post signage with acceptable temperature ranges and corrective actions near storage units.
Have a contingency plan: Power failures, equipment breakdowns or supply chain disruptions can compromise vaccines. Prepare insulated containers, backup generators and alternative storage locations. Conduct Hazard Analysis and Critical Control Points (HACCP) risk assessments to identify critical control points and ensure procedures are documented.
Equipment and supplies checklist
| Article | But | Why you need it |
| Pharmaceutical grade refrigerator | Maintient 2 ° C - 8 ° C; uniform airflow and precise thermostat | Household units may have warm and cold spots; dedicated units prevent excursions |
| Congélateur (–50 °C à –15 °C) | Stores live attenuated vaccines; built in alarms and data logging | Reliable freezers ensure product safety and help meet regulatory requirements |
| Ultra cold freezer or cryogenic shipper | Provides –90 °C to –60 °C or lower for mRNA and gene therapies | Vital for COVID 19 mRNA vaccines and advanced therapies |
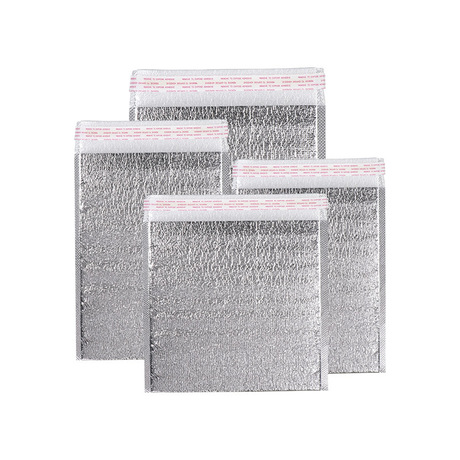
| Matériaux à changement de phase (PCMS) | Stabilize internal temperature by absorbing/releasing heat | Support long distance shipments and minimize thermal shock |
| Panneaux isolés sous vide (Vips) | High performance insulation with thin walls | Increase payload capacity and reduce transportation emissions |
| Enregistreurs de données IoT | Record and transmit temperature and location data in real time | Provide visibility, enable predictive analytics and ensure compliance |
| Backup generator or solar power | Maintains power during outages; solar reduces energy costs | Helps maintain continuous refrigeration and supports sustainability |
Astuces et conseils pratiques
For small clinics: Use purpose built medical refrigerators with built in temperature probes. Avoid storing vaccines in vegetable bins or near freezer coils. Always stock a backup cooler with ice packs and a thermometer in case of power outage.
For mobile vaccination campaigns: Precondition insulated shippers with phase change materials, transport them in refrigerated vehicles and use data loggers to track temperatures. Plan routes to minimize transit time and avoid exposure to extreme climates.
For research laboratories: Dedicate separate freezers for vaccines and reagents; never mix general laboratory materials with vaccine inventory. Maintain an equipment log and schedule preventive maintenance to avoid unexpected failures.
Vraie cas: During the COVID 19 rollout, a rural clinic’s refrigerator lost power. Because the team monitored temperatures with a data logger and had an emergency cooler with ice packs ready, they moved vaccines swiftly into the cooler and prevented spoilage. This simple contingency saved more than 150 doses and ensured community immunisation continued uninterrupted.
How technology is reshaping cold chain vaccine storage in 2025
Cold chain logistics is undergoing rapid transformation driven by digital technologies and sustainability goals. Intelligence artificielle, IoT sensors and blockchain are providing real time visibility and predictive power. AI analytics forecast shipment disruptions, automatically adjust routes and alert operators to potential temperature excursions. Blockchain creates tamper proof records of each handoff, facilitating compliance and recalls.
Leading innovations
| Innovation | Description | Pourquoi ça compte |
| Jumeaux numériques & tours de contrôle | Virtual replicas of cold chain operations monitor shipments and simulate scenarios to optimise routes and energy use | They allow logistics managers to respond swiftly to disruptions and continuously improve processes. |
| Intelligent, emballage durable | Matériaux à changement de phase, panneaux isolés sous vide, RFID smart labels and reusable containers are becoming standard | They extend temperature hold time, reduce waste and support environmental goals. |
| Pôles d'innovation régionaux | Southeast Asia is emerging as a centre for blockchain, solar powered storage and AI assisted logistics | New hubs in Tokyo and Mumbai meet rising demand and shorten supply chains. |
| Strategic mergers & investments | Partnerships like Smurfit Kappa’s merger with WestRock and Sonoco’s acquisition of Eviosys strengthen capabilities | Consolidation accelerates innovation and expands infrastructure. |
| Réutilisable & solutions circulaires | Returnable containers, rental pooling systems and biodegradable foams reduce waste | Circular models lower long term costs and align with ESG mandates. |
| Solar powered storage | Off grid refrigeration uses renewable energy; in the U.S. solar power costs 3.2–15.5 ¢/kWh versus 13.10 ¢/kWh for grid electricity | Reduces reliance on diesel generators and ensures vaccine safety in remote areas. |
Market trends and outlook for 2025
L'industrie de la chaîne du froid est en plein essor. The global cold chain monitoring market is projected to grow from USD 45.19 milliards en 2025 en USD 266.66 milliards 2034 (TCAC ≈ 21.88 %). Le pharmaceutical cold chain packaging market is valued at USD 20.05 milliards en 2025 and expected to reach USD 69.55 milliards 2034. Plus large cold chain packaging is forecast to rise from USD 27.7 milliards en 2025 en USD 102.1 milliards 2034, underscoring the increasing importance of temperature controlled logistics.
Growth drivers include expanding immunisation programmes, rising prevalence of chronic diseases, the advent of mRNA and viral vector vaccines, and the globalisation of direct to patient deliveries. North America currently holds about one third of the market, alors que Asia Pacific is growing fastest, with a projected CAGR of more than 17 %. Sustainability is a key theme: regulators and consumers expect companies to deliver safe products while lowering carbon footprints.
Questions fréquemment posées
Q1: What happens if a vaccine warms above 8 °C?
Vaccine potency declines rapidly when stored outside the recommended range. Proteins may denature, and the vaccine could become ineffective or even harmful. If a temperature excursion occurs, quarantine the affected doses and consult your vaccine manufacturer or local public health authority for guidance.
Q2: Can I use a household refrigerator to store vaccines?
While a household unit may suffice temporarily, it often has significant temperature variation. Pharmaceutical grade refrigerators are designed for vaccine storage, with digital thermostats, alarms and fans that ensure stable conditions. Avoid storing vaccines in door compartments or vegetable bins.
Q3: How often should temperatures be recorded?
CDC guidance recommends checking and recording the minimum and maximum temperatures at least twice daily, at the start and end of each workday. Continuous data loggers provide more granular insight and automated alerts.
Q4: What is the difference between passive and active shipping systems?
Systèmes passifs Utiliser des conteneurs isolés, gel packs or phase change materials to maintain temperature without electricity. They are cost effective and suitable for last mile deliveries. Systèmes actifs incorporate refrigeration or heating units powered by batteries or external power; they offer longer hold times and precise control but are more expensive. Choosing between them depends on distance, payload and temperature requirements.
Q5: How do reusable containers work?
Reusable insulated containers can be cleaned and redeployed multiple times, réduire les déchets et les coûts à long terme. Le marché des emballages réutilisables pour la chaîne du froid devrait passer de USD 4.97 milliards en 2025 en USD 9.13 milliards 2034. Cependant, circular systems require reverse logistics, cleaning protocols and user training.
2025 développements: what’s new in vaccine storage?
Market evolutions
Le medical cold chain storage equipment market, which includes refrigerators, freezers and ultra low temperature systems, était évalué à USD 3.1 milliards en 2024 et devrait atteindre USD 5.2 milliards 2034 à un 5.5 % TCAC. Freezers hold the largest share (environ 37.7 % dans 2024) because live attenuated vaccines and advanced biologics require sub zero temperatures. Demand is propelled by the rise in clinical trials, mass vaccination campaigns and the growth of personalized medicine.
Technological advances
Jumeaux numériques: Logistics platforms now create virtual replicas of storage units and shipping lanes, enabling predictive maintenance and route optimisation.
Analyse prédictive: AI tools such as TransVoyant and CargoSense analyse sensor data to forecast delays and recommend corrective actions, réduire la détérioration.
Smart labels and RFID: Temperature sensitive smart labels with integrated RFID provide continuous monitoring and automate chain of custody records.
Matériaux durables: Bio based foams, aerogels and vacuum insulated panels deliver high thermal efficiency and reduce plastic waste.
Solar powered units: Off grid refrigerators and freezers powered by solar panels ensure reliable vaccine storage in remote areas and reduce operating costs.
Regulatory landscape
Bonnes pratiques de fabrication (GMP) et bonnes pratiques de distribution (PIB) guidelines from agencies like the FDA, European Medicines Agency and WHO govern cold chain operations. New rules require 24 hour traceability, digital documentation and sustainable refrigeration. With the U.S. Loi sur la modernisation de la sécurité alimentaire (FSMA) Règle 204 mandating enhanced traceability for high risk foods by 2026, similar expectations are emerging in vaccine logistics. Companies are deploying blockchain et documentation numérique to create immutable records and facilitate audits.
Résumé et recommandations
Maintenir cold chain vaccine storage is more than keeping a fridge running—it’s a coordinated system that integrates equipment, training and technology to preserve vaccine efficacy. Les principaux points à retenir comprennent:
Adhere to the 2 °C–8 °C standard for most vaccines and respect stricter ranges for frozen and ultra cold products.
Invest in dedicated equipment—pharmaceutical grade refrigerators, freezers and cryogenic shippers—and pair them with phase change materials and data loggers.
Implement robust monitoring and training to detect excursions quickly and empower staff to act.
Tirer parti de la technologie: jumeaux numériques, AI predictive analytics, IoT sensors and blockchain deliver real time visibility and regulatory compliance.
Embrace sustainability and reusability: contenants réutilisables, biodegradable materials and solar powered storage reduce environmental impact and align with market trends.
Plan d'action
Assess your vaccine portfolio: Identify which products are refrigerated, frozen or ultra cold and align equipment accordingly.
Upgrade or calibrate equipment: Ensure refrigerators and freezers meet recommended temperature ranges; install remote monitoring and alarm systems.
Establish a monitoring protocol: Record temperatures twice daily and use data loggers for continuous oversight.
Formez votre équipe: Conduct regular drills on emergency transfers, record keeping and inventory management.
Planifier les imprévus: Prepare backup power sources, insulated transport containers and alternate storage sites.
Explore innovative solutions: Pilot AI based route planning, smart packaging and sustainable materials to stay ahead of regulatory and consumer expectations.
À propos du tempk
Rotation is a leader in cold chain solutions for vaccines, biologics and other temperature sensitive products. We design and manufacture validated insulated containers, portable cryogenic freezers and IoT enabled monitoring systems. Our engineering teams continuously innovate with phase change materials, vacuum insulated panels and sustainable packaging to maintain product integrity from factory to patient. Through a network of logistics partners, technicians and service centres across multiple continents, we help clients comply with GMP/GDP guidelines, réduire les déchets et protéger la santé des patients.
Need help optimising your vaccine cold chain? Talk to our experts for a personalised assessment and discover how smart packaging and data driven tools can elevate your operations.