Gestion de la chaîne du froid des vaccins: Comment assurer la sécurité des vaccins
Mis à jour: 26 novembre2025
Efficace gestion de la chaîne du froid des vaccins est l’épine dorsale d’une vaccination sûre. Sans contrôle et surveillance rigoureux de la température, les vaccins peuvent perdre leur efficacité bien avant d’atteindre votre clinique. La plupart des vaccins doivent être conservés entre 2 °C et 8°C tout au long de la production, transports et administration. L'Organisation mondiale de la santé prévient que jusqu'à 50 % de vaccins sont gaspillés dans le monde en raison d'une logistique inadéquate de la chaîne du froid. Dans ce guide, vous apprendrez à concevoir, gérer et optimiser les chaînes du froid des vaccins pour protéger la santé publique, se conformer aux réglementations et s’adapter aux tendances émergentes 2025.

Pourquoi la gestion de la chaîne du froid des vaccins est importante – comprendre à quel point les plages de température sont étroites, les ingrédients sensibles à la congélation et l’exposition à la chaleur affectent l’efficacité du vaccin et pourquoi les mauvaises chaînes du froid entraînent un gaspillage élevé.
Comment construire une chaîne du froid solide pour les vaccins – explorez les composants essentiels comme les réfrigérateurs spécialement conçus, emballage isolé, enregistreurs de données numériques et personnel formé.
Que faire lorsque les températures s'écartent – apprendre les procédures d’urgence, pratiques de documentation et protocoles d’assurance qualité pour les excursions de température.
Quelles innovations façonnent la gestion de la chaîne du froid dans 2025 – découvrir des tendances telles que l’automatisation, durabilité, suivi en temps réel, intelligence artificielle et concept de chaîne à température contrôlée.
Questions fréquemment posées sur la gestion de la chaîne du froid des vaccins – obtenez des réponses concises sur les plages de stockage, surveillance, Technologie IoT, intervention d'urgence et nouvelles solutions.
Pourquoi la gestion de la chaîne du froid des vaccins est-elle essentielle à la puissance?
Réponse directe
La gestion de la chaîne du froid des vaccins garantit que les vaccins restent dans la plage de température prescrite, généralement 2 °C à 8 °C, du fabricant au patient, prévenir une dégradation irréversible. Composants biologiques des vaccins : protéines, les peptides ou les brins d'ARNm - sont fragiles et perdent rapidement leur efficacité lorsqu'ils sont exposés à la chaleur ou au gel. De mauvaises pratiques en matière de chaîne du froid entraînent une perte d’efficacité et peuvent déclencher des rappels coûteux ou des campagnes de revaccination..
Explication élargie
Imaginez laisser de la glace dans le coffre de votre voiture par une chaude journée: même si tu le recongeles plus tard, la texture et le goût changent. Les vaccins se comportent de la même manière. Ils contiennent des molécules délicates qui se décomposent lorsque les températures dérivent en dehors de la fenêtre recommandée.. L'exposition à la chaleur supérieure à 8°C accélère la dégradation des composants actifs, alors que une congélation en dessous de 0°C peut endommager de façon permanente les vaccins sensibles au gel contenant des adjuvants à base d'aluminium. Contrairement à la nourriture avariée, vous ne pouvez pas voir ou sentir un vaccin compromis; la surveillance continue est le seul indicateur fiable de la qualité. Sans une bonne gestion, vous risquez d’administrer des doses inefficaces, gaspiller des ressources et mettre en péril l’immunité de la communauté. Dans 2025, avec des chaînes d’approvisionnement mises à rude épreuve par les campagnes mondiales de vaccination, les pratiques robustes de la chaîne du froid sont devenues non négociables.
Comprendre les exigences et les catégories de température des vaccins
Les vaccins entrent dans plusieurs catégories de températures en fonction de leur formulation et de leur stabilité. Vaccins de routine contre la rougeole, le tétanos ou l'hépatite B restent stables lorsqu'ils sont réfrigérés à 2 °C–8°C. Les vaccins à base d'ARNm et certaines thérapies géniques nécessitent stockage ultra faible, souvent entre −90°C et −60°C, pour protéger les acides nucléiques fragiles. Vaccins thermostables émergents approuvés pour la chaîne à température contrôlée (CTC) l'utilisation peut tolérer des conditions ambiantes allant jusqu'à 40 °C pendant trois jours. Comprendre ces catégories vous aide à choisir un équipement et un emballage adaptés.
| Catégorie de température | Gamme typique | Exemples de vaccins | Importance |
| Réfrigéré | 2 °C–8°C | Rougeole, hépatite B, TPD | Maintient l’efficacité de la plupart des vaccinations de routine et réduit le gaspillage |
| Congelé | −50°C–−15°C | Vaccins contenant de la varicelle | Stabilité à long terme; nécessite des congélateurs séparés et une manipulation soigneuse |
| Très froid | −90°C–−60°C | vaccins d'ARNm (Par exemple, certains vaccins COVID 19) | Préserve les molécules d’ARNm fragiles et prend en charge la distribution mondiale |
| CTC (Ambiant) | Jusqu'à +40°C pour une durée limitée | Vaccins thermostables sélectionnés | Permet une seule excursion ambiante pendant les campagnes, réduire les charges logistiques |
Astuces et conseils pratiques
Dans les cliniques éloignées: Investir dans alimenté par l'énergie solaire, réfrigérateurs spécialement conçus maintenir une température entre 2 °C et 8 °C même lorsque l’électricité n’est pas fiable. Choisissez des unités avec des batteries internes et des compresseurs économes en énergie.
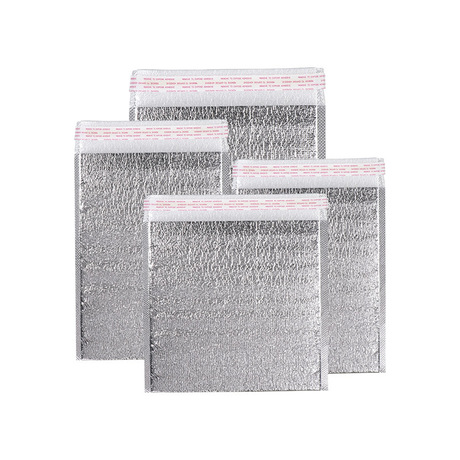
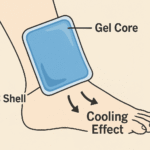
Pendant le transport: Utiliser conteneurs isothermes avec matériaux à changement de phase qui maintiennent des températures sûres pendant au moins 72 heures. Préconditionner les packs à la bonne température et éviter d’ouvrir les conteneurs inutilement.
Dans les pharmacies communautaires: Installer enregistreurs de données numériques avec fonctions d'enregistrement et d'alarme en continu. Choisissez des appareils qui fournissent des alertes à distance par SMS ou par e-mail afin de pouvoir agir rapidement en cas d'excursion de température..
Cas du monde réel: Un centre de santé rural en Afrique de l’Est a mis en place des réfrigérateurs à énergie solaire et des capteurs de température IoT. En recevant des alertes chaque fois que les températures dérivent, le personnel est intervenu rapidement en déplaçant les vaccins vers des refroidisseurs de secours ou en remplaçant l'équipement défectueux. Cette approche proactive a réduit le gaspillage de vaccins de près de 30 % en un an et a amélioré la confiance de la communauté dans les services de vaccination..
Comment construire un système robuste de chaîne du froid pour les vaccins 2025
Réponse directe
Une chaîne du froid robuste pour les vaccins intègre des équipements de stockage spécialisés, emballage approprié, surveillance continue, personnel formé et planification d’urgence. Les réfrigérateurs et congélateurs spécialement conçus maintiennent les températures requises, les emballages isothermes et les matériaux à changement de phase protègent les vaccins pendant le transport, et les enregistreurs de données numériques fournissent des enregistrements continus de température. La formation du personnel et des procédures opérationnelles standard claires garantissent une gestion cohérente et une réponse rapide à tout écart..
Explication élargie
Construire une chaîne du froid pour les vaccins, c'est comme orchestrer une symphonie: chaque instrument doit jouer en harmonie. Unités de stockage sont le fondement. Les États-Unis. Centres de contrôle et de prévention des maladies (CDC) recommande des réfrigérateurs et des congélateurs spécialement conçus ou de qualité pharmaceutique qui maintiennent 2 °C–8°C pour les vaccins réfrigérés et −50°C à −15°C pour les vaccins congelés. Évitez les réfrigérateurs de style dortoir car ils présentent des fluctuations de température et risquent de geler..
Appareils de surveillance de la température (TMD) sont tes yeux et tes oreilles. Les directives de l'OMS stipulent que les vaccins doivent être surveillés en permanence à tous les niveaux de la chaîne d'approvisionnement.. Les enregistreurs de données numériques enregistrent les températures toutes les quelques minutes et fournissent des alertes lorsque les seuils sont dépassés. Dans 2025, de nombreux prestataires logistiques associent des capteurs à plateformes blockchain, créer des enregistrements de température immuables et améliorer la traçabilité.
Solutions d'emballage viens ensuite. Les conteneurs d'expédition isolés doublés de matériaux à changement de phase ou de neige carbonique maintiennent des températures stables pendant le transport.. Pour les vaccins de routine, des packs de gel conditionnés entre 2°C et 8°C suffisent. Les expéditions ultra froides utilisent de la neige carbonique ou de l'azote liquide. L'emballage doit minimiser les espaces d'air, limiter le transfert de chaleur et inclure des indicateurs de température ou des moniteurs de flacons de vaccins.
Transport il s'agit de camions frigorifiques, avion cargo avec conteneurs climatisés et véhicules pré-refroidis. La planification d’itinéraire est importante: des temps de transit plus courts réduisent l’exposition aux conditions extérieures. Lors de la livraison du dernier kilomètre, veiller à ce que les véhicules restent fermés et ombragés, et que les glacières ne soient pas exposées à la lumière directe du soleil.
Personnes et procédures coller le système ensemble. Désigner un coordonnateur des vaccins responsable de la commande, recevoir, stockage et suivi des vaccins. Former tout le personnel impliqué dans la vaccination à suivre les procédures opérationnelles standard (Sops) pour les manipulations courantes et les urgences. Examiner les SOP chaque année et les mettre à jour lors de l'ajout de nouveaux vaccins ou équipements.
Le rôle de l’IoT et de la surveillance en temps réel dans la chaîne du froid des vaccins
L'Internet des objets (IoT) a transformé la gestion de la chaîne du froid d'un processus à forte intensité de main-d'œuvre en un processus automatisé, système proactif. Dispositifs de suivi en temps réel utiliser des capteurs pour surveiller la température, exposition à l'humidité et à la lumière toutes les minutes. Ils envoient des alertes lorsque les seuils sont dépassés et enregistrent les données pour assurer la conformité.. Dans 2025, Les plateformes IoT s'intègrent à intelligence artificielle (IA) pour prédire les pannes potentielles d'équipement et les retards d'itinéraire avant qu'ils ne surviennent. L'IA analyse les données historiques et les prévisions météorologiques pour recommander des itinéraires et des matériaux d'emballage optimaux, réduisant à la fois la détérioration et les émissions.
Astuces et conseils pratiques
Grands hôpitaux: Intégrez des capteurs de température IoT au système d’information de votre hôpital. Les tableaux de bord centraux permettent aux administrateurs de visualiser toutes les unités de stockage, recevoir des alertes et coordonner la maintenance.
Prestataires logistiques: Utiliser analyse prédictive pour optimiser les itinéraires. L'IA peut prévoir le trafic, performances météorologiques et des équipements, suggérer des itinéraires alternatifs ou des packs de glace carbonique supplémentaires pour éviter les excursions de température.
Champions du développement durable: Investir dans emballage réutilisable fabriqué à partir de matériaux biodégradables ou d’isolant recyclable. Les solutions durables pour la chaîne du froid réduisent les déchets et répondent à des réglementations environnementales plus strictes.
Cas du monde réel: Un programme national de vaccination a adopté des enregistreurs de données compatibles avec la blockchain pour les expéditions de vaccins. L’historique des températures de chaque expédition a été enregistré en temps réel. Si un capteur détecte un écart, une alerte automatisée a informé l'établissement de santé le plus proche de préparer un stockage de sauvegarde. Plus de 12 mois, le programme a permis de réduire de 40 % les écarts de température et d'améliorer la transparence lors des audits.
Gérer les excursions de température et assurer la conformité
Réponse directe
Lorsqu'une excursion de température se produit, action immédiate, la documentation et la quarantaine sont essentielles. Les vaccins exposés doivent être étiquetés « Ne pas utiliser," Séparé dans l'unité de stockage et évalué pour sa viabilité. Les établissements doivent informer leur coordonnateur des vaccins, documenter l'incident, mettre en œuvre des procédures d’urgence et consulter leur programme de vaccination ou leur fabricant pour obtenir des conseils.
Explication élargie
Malgré des contrôles rigoureux, pannes de courant, les pannes d'équipement et les erreurs humaines peuvent entraîner des excursions de température. Le CDC conseille de vérifier et d'enregistrer températures minimales et maximales au début de chaque journée de travail. Si vous utilisez un appareil sans affichage min/max, enregistrer la température actuelle au moins deux fois par jour. Les journaux de surveillance doivent inclure la date, temps, personne enregistrant, températures et éventuelles actions correctives.
Lorsqu'un écart est détecté:
Notifier immédiatement le coordonnateur ou le superviseur des vaccins.
Quarantaine les vaccins concernés en les étiquetant « DoNotUse » et en les plaçant dans un conteneur séparé au sein de l’unité de stockage appropriée; ne les jetez pas tant que le fabricant ou l'autorité sanitaire n'a pas déterminé leur viabilité..
Document l'événement à fond, noter la durée de l'excursion, températures enregistrées et mesures prises.
Mettre en œuvre des SOP pour les urgences, ce qui peut inclure le déplacement des vaccins vers une unité de secours, ajuster les paramètres du thermostat ou appeler la maintenance.
Consulter votre programme de vaccination ou votre fabricant de vaccins pour décider de continuer à utiliser ou de jeter les vaccins. Les organismes de réglementation peuvent exiger des enregistrements complets de température pour les audits.
Entraînement est tout aussi vital. Le personnel doit savoir comment utiliser les appareils de surveillance, interpréter les alarmes et réagir rapidement. Formation continue, des cours de remise à niveau annuels et des évaluations de compétences garantissent le bon suivi des procédures.
Procédures opérationnelles standard pour les excursions de température
La standardisation de votre réponse réduit la confusion lorsque chaque seconde compte. Les SOP devraient couvrir:
Entretien des équipements – planifier l’étalonnage et l’entretien réguliers des réfrigérateurs, congélateurs et enregistreurs de données. Gardez les pièces de rechange et les unités de secours à portée de main.
Alimentation de secours – installer des générateurs ou des batteries de secours pour maintenir le contrôle de la température pendant les pannes. Testez ces systèmes tous les trimestres.
Stockage alternatif – pré-identifier les installations à proximité ou les glacières mobiles où les vaccins peuvent être temporairement stockés.
Protocoles de communication – désigner des contacts auprès des services de santé locaux et des fabricants. Assurez-vous que tout le monde sait qui appeler lorsque des excursions ont lieu.
Astuces et conseils pratiques
Lors de pannes de courant: Ne pas ouvrir les portes des unités de stockage. Connectez les générateurs rapidement et vérifiez que les températures reviennent à des plages sûres.. Utilisez des compresses froides ou de la neige carbonique uniquement si cela est recommandé par le fabricant..
Lorsque les capteurs déclenchent une alarme: Vérifiez l'emplacement de l'appareil : les sondes du thermomètre doivent être à l'intérieur du compartiment de rangement., loin des bouches d'aération et des portes. Si l'alarme persiste, documenter la lecture et isoler les vaccins.
Après l'incident: Examinez vos journaux et SOP pour identifier les causes profondes. Mettre en œuvre des actions correctives, comme le réglage des paramètres du thermostat ou la formation du personnel.
Cas du monde réel: Une clinique urbaine a connu une panne de réfrigérateur pendant la nuit. Grâce à une surveillance continue, le personnel a reçu une alerte à minuit. Ils ont transféré les vaccins vers une unité de secours en 30 minutes., a documenté l'excursion et contacté le fabricant. Après tests de qualité, la plupart des vaccins ont été autorisés à être utilisés. Le plan d’urgence de la clinique a permis d’éviter la perte potentielle de milliers de doses et de maintenir la confiance des patients.
2025 Tendances et innovations de la chaîne du froid des vaccins
Présentation des tendances
Le paysage de la chaîne du froid des vaccins évolue rapidement. Dans 2025, les experts du secteur mettent en évidence plusieurs tendances qui conduisent à des améliorations de l’efficacité, durabilité et résilience:
Automatisation et robotique – Les installations de stockage frigorifique adoptent des systèmes automatisés de stockage et de récupération et des robots de manutention. Ces machines fonctionnent 24 heures sur 24, réduire les coûts de main d'œuvre, améliorer la précision et fournir un contrôle constant de la température. Avec environ 80 % d'entrepôts encore non automatisés, le potentiel de croissance est important.
La durabilité comme valeur fondamentale – Systèmes de réfrigération économes en énergie, sources d'énergie renouvelables et emballage biodégradable ou recyclable sont désormais indispensables. La chaîne du froid alimentaire mondiale contribue à environ 2 % des émissions mondiales de CO₂, inciter les entreprises à adopter des pratiques durables.
Visibilité de bout en bout – Les dispositifs de suivi compatibles IoT fournissent un aperçu en temps réel de l'emplacement, température et humidité. Cette visibilité permet aux prestataires logistiques d'optimiser les itinéraires, éviter la détérioration et répondre aux exigences réglementaires.
Moderniser les infrastructures – Investissements dans la réfrigération moderne, une isolation améliorée et des énergies renouvelables sur site aident les installations vieillissantes à répondre aux normes d'efficacité et de durabilité.
IA et analyse prédictive – L’intelligence artificielle analyse les données historiques et en temps réel pour prédire les pannes d’équipements, prévoir la demande et optimiser les itinéraires. Les modèles prédictifs recommandent quand réapprovisionner en neige carbonique ou ajuster les calendriers de livraison, réduire les risques et les coûts.
Croissance de la chaîne du froid pharmaceutique – Le secteur pharmaceutique stimule l’expansion de la logistique de la chaîne du froid. Environ 20 % de nouveaux médicaments sont des thérapies géniques ou cellulaires nécessitant un stockage ultra froid. Le marché mondial de la chaîne du froid pharmaceutique devrait atteindre 65 milliards de dollars américains 2025 et double par 2034.
Partenariats stratégiques et intégration – Collaboration entre fabricants, les prestataires logistiques et les entreprises technologiques améliorent la visibilité et la résilience. La standardisation des données et les conteneurs intelligents permettent une intégration transparente dans les chaînes d'approvisionnement, avec 74 % de données logistiques qui devraient être standardisées d'ici 2025.
Chaîne à température contrôlée (CTC) – L’approche CTC de l’OMS permet de conserver certains vaccins thermostables à des températures ambiantes allant jusqu’à 40 ° C pour une durée limitée avant l'administration. Cette stratégie réduit la dépendance au transport réfrigéré dans les zones reculées et soutient les campagnes de vaccination de masse..
Derniers développements en un coup d'œil
Chambre froide robotisée: Les systèmes automatisés réduisent les erreurs humaines et augmentent le débit, fournissant un contrôle constant de la température et permettant 24/7 opérations.
Emballage écologique: Les entreprises se tournent vers isolation biodégradable et matériaux à changement de phase réutilisables, réduire les déchets et les émissions de carbone.
Maintenance prédictive: L'IA surveille les équipements pour planifier la maintenance avant que des pannes ne surviennent, minimiser les temps d'arrêt et éviter les excursions.
Congélateurs ultra bas: Les nouveaux congélateurs à ultra basse température consomment moins d’énergie et traitent plus efficacement les vaccins à ARNm, soutenir le développement des thérapies géniques.
Transparence de la blockchain: Des enregistrements de température immuables renforcent la confiance avec les régulateurs et les donateurs, assurer la responsabilité tout au long du parcours vaccinal.
Insistance au marché
Le marché de la chaîne du froid continue de se développer. Le secteur de la chaîne du froid pharmaceutique devrait dépasser 65 milliards de dollars américains 2025. La croissance est tirée par les vaccins, produits biologiques et thérapies géniques et cellulaires personnalisées, dont beaucoup nécessitent des conditions ultra froides ou hautement contrôlées. Avec près de 20 % de nouveaux médicaments exigeant un tel stockage, investissement dans les infrastructures, une surveillance avancée et des technologies durables sont essentielles. En même temps, l'infrastructure de la chaîne du froid représente actuellement environ 2% des émissions mondiales de CO₂, créer une pression pour adopter des systèmes économes en énergie. Les entreprises qui équilibrent contrôle strict de la température et durabilité seront les leaders du marché au cours de la décennie à venir..
Questions fréquemment posées
Q1: À quelle plage de température les vaccins doivent-ils être conservés pendant le stockage et le transport?
La plupart des vaccins de routine doivent être administrés entre 2 °C et 8°C de la fabrication à l'administration. Certains vaccins nécessitent des conditions extrêmement froides : les vaccins COVID 19 à base d'ARNm, par exemple, peut avoir besoin d'être stocké à −70°C à −60°C. Suivez toujours la température spécifiée par le fabricant et surveillez en permanence.
Q2: Pourquoi les chaînes du froid des vaccins sont-elles différentes des chaînes réfrigérées générales?
Les chaînes du froid des vaccins maintiennent une plage de température étroite et sont surveillées en permanence car les composants biologiques se dégradent rapidement lorsqu'il est exposé à la chaleur ou au gel. Les chaînes du froid alimentaire tolèrent des gammes plus larges et se concentrent sur la prévention de la détérioration. Les chaînes du froid des vaccins nécessitent également un emballage spécialisé, manipulation minutieuse, et documentation réglementaire.
Q3: Comment les capteurs IoT aident-ils à maintenir la chaîne du froid des vaccins?
Les capteurs IoT enregistrent les températures en temps réel et envoient des alertes lorsque les seuils sont dépassés. Ils créent des journaux de données continus dont les régulateurs ont besoin et intègrent l'IA pour prédire les problèmes avant qu'ils ne surviennent.. Cette approche proactive réduit le gaspillage, optimise les itinéraires et améliore la conformité.
Q4: Que dois-je faire si la température de mon réfrigérateur à vaccins dépasse les limites ??
Étiquetez immédiatement les vaccins « Ne pas utiliser," Mettez-les en quarantaine et informez le coordinateur des vaccins. Documenter l'incident, enregistrer toutes les températures, et suivez vos SOP d'urgence. Contactez votre programme de vaccination ou le fabricant pour déterminer si les vaccins restent viables.
Q5: Quelles innovations façonnent la gestion de la chaîne du froid des vaccins en 2025?
Les innovations clés incluent automatisation et robotique, emballage durable, suivi en temps réel, Analyse prédictive basée sur l'IA, infrastructure modernisée, et le chaîne à température contrôlée approche. Ces technologies améliorent l'efficacité, réduire les déchets et soutenir les campagnes de vaccination à distance.
Résumé et recommandations
Principaux à retenir
Le contrôle de la température est essentiel – Les vaccins doivent rester dans leur plage de température spécifiée (généralement 2 °C à 8 °C) conserver sa puissance. Le gel et la chaleur peuvent endommager les vaccins de façon permanente.
Une surveillance continue évite le gaspillage – Les enregistreurs de données numériques fournissent des enregistrements et des alertes de température en temps réel, veiller à ce que les écarts soient détectés tôt.
Une infrastructure robuste est importante – Des unités de stockage spécialement conçues, emballage isolé, un personnel formé et des SOP claires créent une chaîne du froid fiable.
La préparation aux situations d’urgence permet d’économiser des doses – Mettre en quarantaine les vaccins concernés, documenter les excursions et consulter des experts avant de les jeter.
L’innovation est moteur d’amélioration – Automatisation, durabilité, L'IoT et l'IA transforment la logistique de la chaîne du froid, tandis que les stratégies du CTC élargissent l'accès dans les zones reculées.
Plan d'action
Auditez votre chaîne du froid existante: Évaluer les équipements de stockage, protocoles d'emballage, dispositifs de surveillance et SOP. Identifiez les lacunes et investissez dans des réfrigérateurs spécialement conçus, congélateurs et surveillance continue.
Mettre en œuvre la surveillance de l'IoT: Déployez des capteurs qui fournissent des données de température et de localisation en temps réel. Intégrez ces systèmes à l’IA pour prédire les besoins de maintenance et optimiser les itinéraires.
Élaborer et répéter des SOP: Créer des procédures claires pour les manipulations de routine et les urgences. Former le personnel chaque année et maintenir des listes de contacts à jour pour les fabricants et les autorités sanitaires.
Adopter des pratiques durables: Transition vers une réfrigération économe en énergie, des emballages biodégradables et des sources d'énergie renouvelables pour réduire votre empreinte carbone et répondre aux attentes réglementaires.
Restez informé des tendances: Suivre les évolutions en matière d'automatisation, analyse prédictive, CTC et évolutions réglementaires pour maintenir la compétitivité de votre chaîne du froid.
À propos du tempk
Tempk est l'un des principaux fournisseurs de solutions de chaîne du froid dédiées à la préservation de l'intégrité des produits sensibles à la température.. Nous concevons systèmes de réfrigération spécialement conçus, emballage isolé et Appareils de surveillance compatibles IoT adapté aux besoins du secteur pharmaceutique, industries biotechnologiques et alimentaires. Notre centre de recherche et développement se concentre sur les matériaux durables et les technologies économes en énergie., permettre aux clients de réduire leurs déchets et leurs émissions de carbone. Avec une solide expérience en matière de soutien aux campagnes mondiales de vaccination et à la logistique des sciences de la vie, nous aidons nos partenaires à livrer en toute sécurité, des vaccins puissants dans le monde.
Étapes suivantes: Découvrez comment les solutions Tempk peuvent améliorer la chaîne du froid de vos vaccins. Contactez nos experts pour une évaluation personnalisée et découvrez les outils qui assureront la sécurité de vos vaccins 2025 et au-delà.