Cara Memelihara a Protokol RBC Rantai Dingin di dalam 2025?
Mempertahankan a sel darah merah rantai dingin (RBC) protokol memastikan bahwa darah yang disumbangkan mencapai pasien dengan potensi dan keamanan maksimum. Di dalam 2025, pedoman menetapkan bahwa sel darah merah harus disimpan di 1–6 °C dan diangkut pada 1–10 ° C., dengan batasan waktu dan ketertelusuran yang ketat. Gagal memenuhi batasan ini dapat menyebabkan hemolisis, pertumbuhan bakteri atau hilangnya kapasitas membawa oksigen. Dengan Amerika Serikat saja yang melakukan transfusi lebih dari 29 000 unit sel darah merah setiap hari, rantai dingin yang dikelola dengan baik melindungi pasien dan memastikan pasokan darah yang langka tidak terbuang sia-sia. Panduan ini menyatukan peraturan-peraturan terkini, praktik terbaik dan inovasi pada Desember 2025 untuk membantu Anda menerapkan protokol RBC yang andal.
Artikel ini akan menjawab:
Kisaran suhu berapa yang membuat sel darah merah tetap hidup? Pelajari penyimpanan yang tepat (1–6 °C) dan transportasi (1–10 ° C.) suhu yang ditentukan oleh regulator utama.
Berapa lama sel darah merah dapat disimpan dan diangkut? Pahami batas umur simpan, aturan 30 menit/60 menit dan kebijakan pengembalian.
Peralatan dan sistem pemantauan apa yang diperlukan? Temukan pengaturan lemari es, Data Loggers, pengirim dan sistem alarm yang tervalidasi.
Standar mana yang mengatur kepatuhan? Bandingkan FDA, JPAC, Pedoman WHO dan UE, dan mempelajari cara mempersiapkan audit.
Bagaimana tren teknologi dan pasar membentuk kembali rantai dingin? Jelajahi sensor IoT, bahan perubahan fase, drone, blockchain dan inisiatif keberlanjutan.
Apa Persyaratan Suhu Inti untuk Sel Darah Merah?
Jawaban Langsung
Sel darah merah harus disimpan pada suhu 1–6 °C dan disimpan antara 1–10 °C selama pengangkutan. Regulator utama menyetujui rentang sempit ini karena penyimpangan dapat mempercepat hemolisis atau memungkinkan bakteri berkembang biak. AS. Administrasi Makanan dan Obat -obatan (FDA) mengamanatkan penyimpanan di 1–6 °C dan pendinginan terus menerus menuju 1–10 ° C. selama pengiriman. Layanan Darah Kanada mencatat bahwa komponen sel darah merah harus tetap sama 1–6 °C selama penyimpanan, dan sistem transportasi memungkinkan perluasan yang lebih luas 1–10 ° C. rentang waktu transit di bawah 24 jam. Di Australia, program Lifeblood menentukan 2–6 °C untuk penyimpanan dengan umur simpan hingga 42 hari -hari. Pedoman JPAC Jepang menetapkan suhu inti 4 ± 2 ° C. dan izinkan satu perjalanan hingga 10 ° C. selama kurang dari lima jam.
Penjelasan yang diperluas
Menjaga sel darah merah dalam kisaran ini akan menjaga integritas dan kapasitas membawa oksigen. Jika suhu turun di bawah batas bawah, kristal es dapat merusak membran sel; jika melebihi batas atas, aktivitas metabolisme meningkat dan mengurangi umur simpan. A 2020 Studi transfusi rumah dari Jepang menunjukkan bahwa transportasi mobil tidak memadai (menggunakan pendingin yang tidak divalidasi) menyebabkan peningkatan kadar laktat dehidrogenase—penanda hemolisis—sementara unit diangkut pada 2–6 °C dalam lemari es yang tervalidasi tetap menjaga kualitasnya. Kerangka peraturan dari FDA, Badan Obat Eropa (Ema), Organisasi Kesehatan Dunia (SIAPA) dan lembaga nasional seperti JPAC menstandarkan rentang ini untuk melindungi pasien.
Pemantauan Harian dan Sistem Alarm
Pemantauan berkelanjutan sangat penting untuk memastikan suhu tetap dalam kisaran yang ditentukan. Lemari es penyimpanan darah sebaiknya memiliki kipas yang terpasang untuk sirkulasi dan pemeliharaan udara 1–6 °C seragam. FDA dan AABB merekomendasikan penggunaan grafik perekam listrik atau Data Loggers rekor suhu itu setidaknya setiap empat jam. Bank darah modern mempekerjakan Sensor IoT yang mencatat data setiap dua menit dan memicu peringatan jika suhu berubah, memungkinkan staf untuk merespons sebelum hemolisis terjadi. Setiap kulkas juga harus memilikinya termometer referensi internal ditempatkan di rak tertinggi dan terendah untuk mendeteksi stratifikasi. Alarm harus diuji secara berkala dan didokumentasikan; setiap variasi atau kelalaian suhu harus dijelaskan, inisial dan diberi tanggal.
Meja 1 – Kisaran Suhu berdasarkan Kerangka Peraturan
| Kerangka | Kisaran suhu | Fokus Utama | Implikasi Praktis |
| FDA (21 CFR § 640) | Simpan sel darah merah di 1–6 °C; transportasi di 1–10 ° C. | Menetapkan minimum AS. persyaratan pengumpulan dan pemrosesan darah | Pertahankan lemari es pada suhu 1–6 °C dan gunakan kotak atau pendingin yang memenuhi syarat dengan kantong es untuk menjaga unit tetap di bawah suhu tersebut 10 °C selama pengiriman. |
| JPAC (Inggris) | Suhu penyimpanan inti 4 ± 2 ° C., satu tamasya hingga 10 ° C. selama ≤5 jam; suhu permukaan pengangkutan 2–10 ° C. | Panduan terperinci untuk Inggris. layanan darah | Validasi kontainer transit; jika unit menghangat di atas 10 ° C untuk >5 jam, karantina atau buang. |
| SIAPA | Pertahankan suhu yang benar mulai dari donasi hingga transfusi | Menekankan standar global dan manajemen kualitas | Perlakukan sel darah merah sebagai obat yang sensitif terhadap suhu—pemantauan berkelanjutan dan sistem kualitas sangat penting. |
| Studi transfusi di rumah (Jepang) | Simpan dan transportasi di 2–6 °C; menghindari osilasi dan penempatan vertikal | Menyoroti risiko selama transportasi mobil atau drone | Tempatkan tas secara horizontal dan kencangkan untuk meminimalkan hemolisis akibat getaran selama pengangkutan. |
| 30Aturan Menit/60 Menit (JPAC) | Unit yang dikeluarkan dari penyimpanan terkontrol harus dikembalikan di dalamnya 30 menit; jika keluar untuk 30–60 menit, karantina untuk 6 jam sebelum diterbitkan ulang | Mencegah perubahan suhu berulang kali di dalam rumah sakit | Labeli unit dengan waktu penerbitannya; karantina mereka yang melebihi batas dan dokumen. |
Tabel tersebut menggambarkan bahwa meskipun regulator menyetujui hal tersebut 1–6 °C/1–10 ° C. prinsip, pedoman nasional menyempurnakan batas waktu dan tunjangan perjalanan. Anda harus mengintegrasikan aturan paling ketat yang berlaku ke dalam protokol Anda untuk memastikan kepatuhan.
Cara Menangani Operasi Penyimpanan dan Transportasi RBC?
Prinsip Inti
Penyimpanan dan transportasi yang aman mendukung setiap protokol rantai dingin. Peraturan FDA mengharuskan sel darah merah disimpan segera setelah diproses di 1–6 °C. Pedoman JPAC memerlukan suhu penyimpanan inti sebesar 4 ± 2 ° C. dan izinkan hanya satu kenaikan suhu hingga 10 ° C. selama kurang dari lima jam. Selama transportasi, Sel darah merah harus disimpan di antara keduanya 2 °C dan 10 ° C. dan kontainer transit harus divalidasi. WHO menekankan bahwa putusnya rantai dingin darah menyebabkan pemborosan dan meningkatkan reaksi transfusi.
Peralatan dan Tata Letak Penyimpanan
Kamar dingin dan lemari es – Gunakan lemari es bank darah yang dibuat khusus dengan kipas untuk mengalirkan udara dingin. Rak atau kompartemen terpisah harus diperuntukkan agar tidak saling bersilangan, cocok silang, unit autologous dan ketinggalan jaman. Termometer internal di bagian atas dan bawah mendeteksi stratifikasi.
Pemantauan suhu dan alarm – Pencatat data berkelanjutan atau grafik perekam listrik harus mencatat suhu setidaknya setiap empat jam. Banyak sistem modern merekam setiap dua menit dan memicu alarm suara ketika batasan dilanggar. Simpan sertifikat kalibrasi dalam arsip dan pastikan monitor divalidasi berdasarkan standar yang diakui seperti NIST atau UKAS.
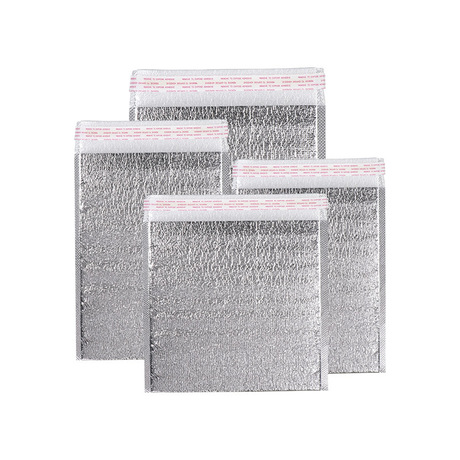
Kontainer pengangkutan yang tervalidasi – JPAC mengamanatkan pengirim untuk menjaga suhu permukaan sebesar 2–10 ° C. Selama transportasi. Ruang udara mati harus diminimalkan, dan es yang mencair tidak boleh langsung bersentuhan dengan kantong darah. Sebelum diisi dengan komponen, kondisikan wadah ke suhu yang diinginkan.
Bahan pengepakan dan pendingin – Pedoman pengiriman komersial mengharuskan sel darah merah ditempatkan dalam kantong plastik anti bocor sekunder di dalam kokoh, wadah terisolasi. Bahan pendingin yang memadai—sebaiknya es basah yang dipotong dadu di atas darah—mempertahankan suhu di bawah 10 °C selama transportasi. Palang Merah Amerika menggunakan kotak berkualitas yang divalidasi untuk menjaga suhu pengiriman yang disyaratkan.
Pencatat data dan ketertelusuran – Untuk pengiriman yang melebihi waktu pengangkutan yang divalidasi, menyertakan pencatat data untuk terus mencatat suhu internal. Jika logger menunjukkan tamasya, mengunduh dan menganalisis data untuk memutuskan apakah produk tetap sesuai.
Durasi Transportasi dan Batas Perjalanan
Sel darah merah memiliki daya tahan terbatas di luar lingkungan yang terkendali. Layanan Darah Kanada menyarankan agar waktu transportasi tidak boleh melebihi 24 jam, menggunakan kontainer pengiriman tervalidasi yang memelihara 1–6 °C. Pedoman JPAC menetapkan bahwa unit dapat tetap berada di luar ruang pendingin hingga 30 menit tanpa karantina; jika keluar untuk 30–60 menit, mereka harus dikarantina setidaknya enam jam sebelum diterbitkan kembali. Unit tidak boleh menjalani lebih dari tiga kunjungan total. Meja 2 merangkum durasi utama dan aturan pengembalian.
Meja 2 – Durasi Penyimpanan dan Aturan Pengembalian
| Parameter | Persyaratan | Sumber | Mengapa itu penting |
| Waktu penyimpanan maksimum | Hingga 42 hari -hari untuk komponen sel darah merah dengan suplementasi adenin; 35 hari -hari ketika disimpan di 4 ± 2 ° C. berdasarkan pedoman JPAC | JPAC & rekomendasi bank darah umum | Mendukung manajemen inventaris sambil menjaga kelangsungan hidup sel. |
| Durasi transportasi | Pertahankan suhu permukaan ≤ 10 ° C. untuk satu kesempatan tidak melebihi 12 jam | JPAC | Transportasi yang lebih lama dapat menyebabkan pemanasan; membatasi paparan memastikan kemasan yang divalidasi tetap efektif. |
| Kembali dari bangsal | Kembali ke dalam 30 menit; jika antara 30–60 menit, karantina untuk 6 jam sebelum diterbitkan ulang | JPAC | Mencegah siklus suhu berulang yang merusak sel darah merah. |
| Transfusi rumah | Menjaga 2–6 °C selama transportasi mobil atau drone; hindari osilasi dan letakkan tas secara horizontal | Studi transfusi di rumah di Jepang | Mengontrol risiko hemolisis selama transfusi di rumah atau jarak jauh. |
Menangani Unit RBC Selama Pengeluaran dan Kepulangan Rumah Sakit
Setelah unit RBC meninggalkan bank darah untuk transfusi, jam dimulai. Dokumentasikan waktu penerbitan dan pastikan unit tetap pada suhu terkendali selama pengangkutan ke bangsal. Jika transfusi tertunda, segera kembalikan unit ke bank darah. Pedoman JPAC menetapkan bahwa jika suatu unit berada di luar penyimpanan terkendali lebih dari 30 menit, itu harus bukan dikembalikan langsung ke lemari es utama tetapi dikarantina setidaknya enam jam sebelum diterbitkan kembali. Dalam situasi apa pun unit tidak boleh menjalani 30hingga 60 menit dari masa penyimpanan lebih dari tiga kali. Selalu selesaikan transfusi dalam waktu empat jam setelah transfusi dikeluarkan untuk mencegah perkembangbiakan bakteri.
Tip Praktis untuk Pengendalian Suhu
Rekomendasi praktis dari regulator dan penelitian terbaru dapat membantu mengurangi risiko:
Gunakan lemari es dan pendingin yang tervalidasi: Hanya peralatan yang dirancang untuk penyimpanan darah yang menjaga keseragaman suhu. KITA. peraturan memerlukan pendinginan terus menerus 1–10 ° C. Selama transportasi, dan Inggris. pedoman menuntut kontainer transit yang divalidasi.
Pantau terus menerus: Pasang pencatat data atau sensor IoT yang mencatat suhu setiap beberapa menit dan memicu peringatan ketika batas dilanggar. Deteksi perubahan halus sebelum hemolisis terjadi.
Minimalkan waktu penanganan: Simpan sel darah merah di luar lingkungan terkendali selama kurang dari 30 menit ketika dikeluarkan ke area klinis. Jika batasnya terlampaui, karantina unit selama enam jam dan dokumentasikan kejadian tersebut.
Arahkan tas dengan benar: Studi transfusi di rumah menunjukkan bahwa penempatan vertikal dan osilasi meningkatkan hemolisis; letakkan tas secara horizontal dan kencangkan selama pengangkutan.
Rencanakan Kontinjensi: Memiliki prosedur jika listrik padam, kerusakan kendaraan dan keterlambatan pengiriman. Dokumentasikan setiap perubahan suhu dan tindakan perbaikan.
Contoh kasus: A 2020 Penelitian di Jepang membandingkan unit RBC yang diangkut dengan mobil menggunakan lemari es transportasi aktif versus kotak pendingin. Unit dalam pendingin yang tidak divalidasi menunjukkan tingkat laktat dehidrogenase yang lebih tinggi, menunjukkan hemolisis, sementara yang diangkut di 2–6 °C dalam lemari es yang tervalidasi tetap terjaga kualitasnya. Kontrol suhu yang tepat dan penempatan kantong secara horizontal sangat penting.
Badan Pengatur dan Standar Mana yang Mengatur Kepatuhan Rantai Dingin RBC?
Peraturan RBC rantai dingin diberlakukan oleh banyak otoritas, dan kepatuhan memerlukan kepatuhan terhadap peralatan yang divalidasi, perangkat pemantauan yang dikalibrasi, dokumentasi rinci, dan pelatihan staf.
Kerangka Peraturan Utama
FDA (21 Bagian CFR 640) – Menentukan penyimpanan di 1–6 °C dan pendinginan terus menerus menuju 1–10 ° C. Selama transportasi. Peralatan harus diperiksa, dan unit abnormal tidak boleh dikeluarkan.
Praktik Distribusi yang Baik (PDB) – Pedoman PDB mencakup pengendalian suhu, keterlacakan, kompetensi staf dan prosedur tertulis. Peraturan ini diakui secara global dan mendasari peraturan nasional. Banyak lembaga nasional mewajibkan kepatuhan terhadap PDB bagi penyedia logistik darah.
Standar Kalibrasi – Perangkat pemantauan suhu harus dikalibrasi terhadap standar yang diakui seperti NIST atau UKAS. Sertifikat kalibrasi harus disimpan dalam arsip.
Lampiran GMP UE 11 & Integritas Data – Sistem elektronik harus memiliki jejak audit, penanganan data yang aman dan perangkat lunak yang divalidasi. Pastikan perangkat lunak pemantauan suhu tahan terhadap kerusakan dan tervalidasi.
Peraturan Uji Klinis UE 536/2014 – Produk obat investigasi, termasuk komponen darah yang digunakan dalam uji klinis, harus mematuhi kontrol suhu dan pencatatan yang terdokumentasi.
JPAC & 30Aturan Menit – Menentukan suhu penyimpanan inti 4 ± 2 ° C. dan membatasi kunjungan di atas 10 ° C.. Peraturan ini juga menetapkan prosedur untuk mengembalikan unit ke tempat penyimpanan atau membuang unit yang melebihi batas waktu.
Manajemen Mutu WHO – Menekankan bahwa otoritas kesehatan nasional harus mendukung layanan darah yang terkoordinasi dengan manajemen kualitas yang kuat di setiap tingkat.
Menavigasi Persyaratan Kepatuhan
Ekspektasi peraturan melampaui target suhu. Pihak berwenang membutuhkan peralatan yang divalidasi, perangkat pemantauan yang dikalibrasi, dokumentasi rinci, pelatihan staf Dan rencana darurat.
Peralatan yang Divalidasi: Kualifikasi ulang lemari es, freezer, pendingin dan kendaraan sebelum digunakan; berkualifikasi ulang setelah perbaikan atau saat memindahkan peralatan.
Dokumentasi & Kalibrasi: Simpan catatan log suhu, sertifikat pemeliharaan dan kalibrasi peralatan. Staf harus mendokumentasikan setiap penyimpangan dan tindakan perbaikan. Pastikan sistem digital tervalidasi dan memiliki jejak audit.
Pelatihan: Penilaian kompetensi tahunan memastikan semua staf memahami batasan suhu, prosedur darurat dan persyaratan dokumentasi.
Daftar periksa: Kembangkan daftar periksa sederhana untuk pengumpulan darah, kemasan, pengiriman dan penerimaan. Daftar periksa standar mengurangi kesalahan dan mendukung kesiapan audit.
Libatkan Laboratorium Kalibrasi: Bekerja sama dengan laboratorium terakreditasi untuk mengkalibrasi sensor dan memastikan akurasi.
Audit: Regulator mengharapkan Anda untuk mempertahankan sertifikat, tindakan perbaikan dan catatan lacak balak. Menyimpan catatan digital setidaknya selama sepuluh tahun, seperti yang direkomendasikan oleh banyak bank darah.
Lulus Audit dengan Dokumentasi yang Benar
Audit fokus pada ketertelusuran dan dokumentasi. Regulator mengharapkan Anda menyajikan catatan suhu, log pemeliharaan peralatan dan laporan penyimpangan. Meja 3 merangkum dokumen-dokumen penting yang diperlukan dalam berbagai kerangka kerja dan langkah-langkah praktis untuk mempersiapkannya.
| Kerangka Peraturan | Dokumen Penting Diperlukan | Langkah Praktis |
| PDB / GxP | Prosedur operasi standar, catatan pelatihan, laporan penyimpangan, dokumen kualifikasi peralatan | Mengembangkan prosedur tertulis untuk penyimpanan, transportasi dan kembali. Lakukan pelatihan penyegaran rutin dan dokumentasikan penyimpangan dengan analisis akar permasalahan. |
| FDA (21 CFR § 640) | Catatan suhu, log pemeliharaan peralatan, catatan donor dan produk | Gunakan pencatat data otomatis dengan jejak audit. Periksa unit secara visual sebelum dikeluarkan dan karantina unit yang penampilannya tidak normal. |
| Lampiran GMP UE 11 | Laporan validasi perangkat lunak, log kontrol akses, ulasan jejak audit | Validasi perangkat lunak pemantauan suhu dan batasi akses ke pengguna yang berwenang. Tinjau jejak audit secara teratur untuk mendeteksi perubahan yang tidak sah. |
| Pedoman JPAC | Catatan perjalanan suhu, log karantina, 30dokumentasi pengembalian menit/60 menit | Beri label unit dengan waktu penerbitan dan lacak waktu pengembalian. Unit karantina yang melebihi 30 menit keluar dari lemari es. |
Penyimpanan dan Transportasi Sel Darah Merah yang Aman: Persyaratan Terperinci
Menyiapkan Ruangan Dingin dan Kulkas
Lemari es bank darah yang dibuat khusus dengan kipas angin memastikan suhu seragam. Simpan rak atau kompartemen terpisah untuk berbagai kategori—tidak saling cocok, cocok silang, unit autologous dan ketinggalan jaman—sehingga kesalahan inventaris tidak mengakibatkan kesalahan transfusi. Tempatkan termometer internal di rak atas dan bawah untuk mendeteksi stratifikasi. Pastikan interior bersih dan penerangan cukup, dan menyimpan catatan tertulis tentang pemeriksaan suhu harian.
Kontainer Transportasi dan Pengepakan
Gunakan pengirim tervalidasi yang memelihara 2–10 ° C. selama transit. Setiap unit harus dimasukkan ke dalam kantong plastik anti bocor sebelum ditempatkan di dalam wadah berinsulasi. Isi ruang udara mati dengan bahan isolasi, dan pastikan paket es atau perubahan fasa telah dikondisikan terlebih dahulu hingga mencapai suhu yang diinginkan. Es harus ditempatkan di atas darah, saat udara dingin bergerak ke bawah, dan volume es untuk jarak jauh setidaknya harus sama dengan volume darah. Saat menggunakan sistem pasif (kotak terisolasi dengan paket PCM), kondisikan terlebih dahulu pendingin ke suhu target untuk menghindari pemanasan mendadak.
Penanganan Selama Penerbitan dan Pengembalian
Itu 30aturan menit sangat penting: unit yang dikeluarkan dari lemari es harus ditransfusikan atau dikembalikan ke dalam 30 menit; jika keluar selama 30–60 menit, karantina selama enam jam sebelum diterbitkan kembali. Beri label pada unit dengan waktu penerbitan dan lacak waktu pengembalian. Minimalkan perpindahan berulang antara bangsal dan bank darah—setiap perjalanan meningkatkan risiko hemolisis. Selesaikan transfusi dalam waktu empat jam setelah dikeluarkan untuk mengurangi perkembangbiakan bakteri.
Tip Praktis untuk Penyimpanan dan Transportasi
Pendingin prasyarat: Dinginkan kontainer transit ke suhu target sebelum memuat unit RBC.
Gunakan bahan pengubah fasa (PCMS): PCM mempertahankan 2–8 ° C. untuk waktu yang lama tanpa daya eksternal dan memberikan stabilitas yang lebih baik dibandingkan paket es saja. Mereka juga meminimalkan risiko pembekuan sel darah merah dan mendukung pengiriman melalui drone.
Orientasi RBC yang aman: Penempatan tas secara horizontal mengurangi hemolisis akibat getaran selama pengangkutan dengan mobil atau drone.
Periksa aturan 30 menit: Simpan pengatur waktu pada setiap unit yang dikeluarkan dan tandai unit yang melebihi batas; karantina mereka sebagaimana mestinya.
Rekam semuanya: Dokumentasikan suhu pada saat pengiriman dan penerimaan; menjaga log dapat diakses untuk audit.
Alat Pendukung Keputusan dan Evaluasi Diri
Interaktif kalkulator rantai dingin dapat membantu Anda merencanakan pengiriman. Masukkan jumlah unit, suhu lingkungan dan waktu transit untuk menerima rekomendasi jenis kontainer, Kuantitas PCM dan pencatat data yang diperlukan. A daftar periksa penilaian diri dapat memandu Anda memenuhi persyaratan peraturan—memastikan Anda memiliki peralatan yang tervalidasi, sertifikat kalibrasi, SOP dan catatan pelatihan staf. Alat-alat ini tidak hanya meningkatkan kepatuhan tetapi juga melibatkan pengguna, mengurangi rasio pentalan dan meningkatkan sinyal pengguna.
Inovasi yang Mentransformasikan Rantai Dingin RBC di 2025
Teknologi mengubah cara sel darah merah disimpan dan diangkut. Sensor IoT, bahan perubahan fase, drone, blockchain dan kecerdasan buatan (Ai) bukan lagi konsep futuristik; ini adalah alat praktis untuk memastikan kepatuhan dan mengurangi limbah.
Sensor IoT dan Pemantauan Waktu Nyata
Pasang perangkat IoT ke kantong darah atau wadah transportasi untuk mencatat suhu, kelembaban dan getaran setiap beberapa menit. Pedoman terbaru merekomendasikan sensor dengan chip memori dan dasbor. Saat sistem mendeteksi perubahan suhu, itu memicu peringatan dan memungkinkan tindakan korektif. Data IoT juga mendukung pemeliharaan prediktif—layanan penjadwalan sebelum peralatan rusak—dan memfasilitasi rotasi masuk/keluar pertama berdasarkan umur simpan unit.
Bahan Perubahan Fase (PCMS) dan Pendinginan Pasif
PCM menyerap dan melepaskan energi panas saat mengubah fase. PCM dirancang untuk pemeliharaan transportasi darah 2–8 ° C. untuk waktu yang lama dan memberikan pendinginan yang stabil tanpa listrik. Produk ini menawarkan waktu tahan yang lebih lama dibandingkan kemasan gel tradisional dan meminimalkan risiko pembekuan sel darah merah. Menggabungkan PCM dengan wadah terisolasi dan pencatat data menciptakan sistem pasif kuat yang cocok untuk lokasi terpencil dan pengiriman drone.
Drone dan Logistik Berbantuan AI
Kendaraan udara tak berawak yang dilengkapi dengan paket gel penstabil suhu dan peredam getaran mengantarkan darah dengan cepat ke seluruh wilayah perkotaan dan terpencil. Penjadwalan yang didukung AI memprioritaskan pengiriman berdasarkan umur simpan, urgensi dan jarak. Di dalam 2023, Program di Rwanda dan Ghana menunjukkan bahwa pengiriman darah melalui drone mengurangi pemborosan darah dan mempersingkat waktu pengiriman dengan tetap menjaga kepatuhan. Pertimbangan etis mencakup stabilitas muatan, peraturan wilayah udara dan privasi data.
Peramalan Blockchain dan AI
A 2025 ulasan mencatat bahwa teknologi blockchain mengamankan rantai pasokan darah dengan menyediakan sistem yang terdesentralisasi, buku besar yang tidak dapat diubah untuk melacak sumbangan, kondisi penyimpanan dan catatan transfusi. Kontrak pintar mengotomatiskan pemeriksaan kepatuhan dan berintegrasi dengan model perkiraan AI, yang menganalisis riwayat penggunaan dan faktor demografi untuk memprediksi permintaan darah. Bersama, blockchain dan AI mendukung jadwal pengumpulan proaktif, mengurangi kekurangan dan pengumpulan berlebih.
Ketahanan dan Keberlanjutan Iklim
Peristiwa cuaca ekstrem—gelombang panas, banjir, badai—dapat mengganggu rantai pasokan darah dan meningkatkan permintaan selama bencana. Para peneliti merekomendasikan untuk membangun ketahanan melalui generator cadangan, unit penyimpanan seluler, kendaraan transportasi yang tahan iklim dan bank darah berjalan. Keberlanjutan juga semakin mendapat perhatian: pengirim terisolasi yang dapat didaur ulang, pendingin bertenaga surya dan sistem pengemasan loop tertutup mengurangi dampak lingkungan. Rumah sakit dan penyedia logistik semakin banyak yang mengadopsi teknologi ini untuk menyelaraskan dengan tanggung jawab sosial perusahaan dan ekspektasi peraturan.
Meja 4 – Inovasi dan Manfaatnya
| Inovasi | Keterangan | Bagaimana Ini Membantu Anda |
| Sensor IoT | Pencatat data yang memonitor suhu, kelembaban dan getaran; rekam setiap beberapa menit dan kirim peringatan | Memberikan visibilitas waktu nyata, mencegah kunjungan dan membuat catatan yang dapat diaudit. |
| Bahan Perubahan Fase (PCMS) | Bahan pendingin pasif yang menjaga 2–8 ° C. untuk waktu yang lama | Memperpanjang waktu pengiriman tanpa listrik, mengurangi risiko pembekuan dan menyederhanakan pengemasan. |
| Drone & Penjadwalan AI | UAV dengan pengatur suhu mengalirkan darah dengan cepat; AI memprioritaskan pengiriman berdasarkan umur simpan | Jangkau daerah terpencil dengan cepat, mengurangi pemborosan dan mengoptimalkan sumber daya. |
| Blockchain & Peramalan AI | Buku besar terdesentralisasi melacak donasi dan penyimpanan; Model AI memprediksi permintaan | Meningkatkan ketertelusuran, mengurangi penipuan, meningkatkan perencanaan pasokan dan mengotomatiskan kepatuhan. |
| Tindakan Ketahanan Iklim | Daya cadangan, unit seluler, bank darah berjalan, kemasan berkelanjutan | Menjaga pasokan saat terjadi bencana, mengurangi dampak lingkungan dan memenuhi tujuan keberlanjutan. |
Kiat untuk Mengadopsi Solusi Inovatif
Mulailah dari yang kecil: Uji coba sensor IoT atau PCM pada sejumlah pengiriman terbatas untuk mengevaluasi kinerja sebelum meningkatkannya.
Integrasikan sistem data: Hubungkan data sensor dengan manajemen inventaris dan sistem audit untuk mengotomatiskan peringatan.
Bekerja dengan regulator: Saat mengimplementasikan drone atau blockchain, melibatkan otoritas lokal sejak dini untuk memahami peraturan wilayah udara dan persyaratan privasi data.
Rancang kemasan yang tangguh: Gabungkan pengirim berinsulasi dengan PCM dan peredam kejut untuk melindungi sel darah merah selama penerbangan dan transportasi darat.
Prioritaskan keberlanjutan: Pilih bahan yang dapat didaur ulang dan rencanakan daur ulang di akhir masa pakainya untuk meminimalkan dampak lingkungan.
2025 Tren Pasar dan Wawasan Konsumen
Sektor RBC rantai dingin berkembang pesat. Perkiraan memperkirakan pasar rantai dingin farmasi melebihi $65 miliar masuk 2025 dan akan tumbuh menjadi lebih dari $130 miliar oleh 2034. Lonjakan ini mencerminkan meningkatnya permintaan akan produk biologis, vaksin dan terapi lanjutan yang memerlukan kontrol suhu yang ketat. Dalam pengobatan transfusi, itu Palang Merah Amerika melaporkan bahwa lebih dari 29 000 unit sel darah merah dibutuhkan setiap hari di Amerika Serikat. Dengan populasi yang menua dan operasi yang lebih kompleks, permintaan diperkirakan akan meningkat. Variasi musiman, keadaan darurat kesehatan masyarakat dan peristiwa iklim dapat menyebabkan kekurangan atau kelebihan darah secara tiba-tiba; Perkiraan berbasis AI membantu memuluskan fluktuasi ini.
Perkembangan terbaru
Pertumbuhan permintaan & pergeseran demografi: Populasi yang menua meningkatkan kebutuhan transfusi; lebih banyak operasi elektif dan kasus trauma mendorong konsumsi RBC.
Inisiatif keberlanjutan: Regulator dan konsumen meneliti dampak logistik terhadap lingkungan. Perusahaan mengadopsi pengirim barang yang dapat didaur ulang, pendingin bertenaga surya dan sistem pengemasan loop tertutup.
Transformasi digital: IoT, AI dan blockchain bersatu untuk meningkatkan transparansi dan efisiensi. Data waktu nyata memungkinkan inventaris tepat waktu dan mengurangi pemborosan.
Strategi ketahanan iklim: Cuaca ekstrem mengancam rantai pasokan; rencana darurat termasuk unit penyimpanan seluler, listrik cadangan dan bank darah berjalan.
Pengetatan peraturan: Pertumbuhan ilmu biologi dan terapi gen telah menyebabkan regulator memperkuat persyaratan rantai dingin; mengharapkan lebih banyak tuntutan audit dan dokumentasi.
Wawasan Pasar untuk Penyedia
Rumah Sakit, bank darah dan penyedia logistik harus berinvestasi pada infrastruktur rantai dingin yang kuat dan mengadopsi teknologi modern seperti sensor IoT dan blockchain. Upaya keberlanjutan—menggunakan bahan-bahan yang dapat didaur ulang, peralatan bertenaga surya dan sistem loop tertutup—tidak hanya menjawab pertimbangan etis namun juga membangun tanggung jawab sosial perusahaan dan membedakan layanan Anda. Menjadi yang terdepan dalam tren membantu membangun kepercayaan dengan para donor, pasien dan regulator.
Pertanyaan yang sering diajukan
Q1: Apa perbedaan rantai dingin darah dan rantai dingin vaksin?
Rantai dingin darah mengacu pada proses pengumpulan yang terkontrol, pengolahan, menyimpan dan mengangkut produk darah. Sel darah merah disimpan pada suhu 1–6 °C dan diangkut pada suhu 1–10 °C. Rantai dingin vaksin mempertahankan kisaran 2–8 ° C. untuk sebagian besar vaksin dan –18 °C untuk plasma beku, tetapi komponen darah memiliki persyaratan yang lebih berbeda seperti trombosit pada suhu kamar.
Q2: Berapa lama sel darah merah bisa disimpan?
Berdasarkan pedoman FDA dan JPAC, Sel darah merah yang disimpan dalam larutan tambahan adenin dapat bertahan hingga 42 hari -hari. JPAC memungkinkan penyimpanan untuk 35 hari -hari pada 4 ± 2 ° C. dengan variasi suhu minimal. Selalu periksa tanggal kedaluwarsa dan rotasikan stok sesuai kebutuhan.
Q3: Apa jadinya jika suhu melebihi 6 °C selama pengangkutan?
Kecil, tamasya satu kali terkadang diperbolehkan. Pedoman JPAC mengizinkan satu perjalanan hingga 10 ° C. untuk kurang dari jam lima. Peraturan FDA memerlukan pendinginan 1–10 ° C. Selama transportasi. Jika terjadi tamasya, karantina unit tersebut dan ikuti kebijakan fasilitas Anda untuk memutuskan apakah unit tersebut dapat digunakan.
Q4: Apakah drone aman untuk transportasi darah?
Ya—bila dilengkapi dengan benar. Drone dengan paket gel penstabil suhu, peredam getaran dan pemantauan waktu nyata telah menyalurkan darah dengan cepat dan aman di Afrika dan AS. Namun, kerangka peraturan dan persyaratan izin wilayah udara masih terus berkembang.
Q5: Bagaimana blockchain meningkatkan kepatuhan rantai dingin?
Blockchain menciptakan catatan abadi tentang perjalanan setiap unit darah mulai dari donasi hingga transfusi. Ini melacak kondisi penyimpanan, lokasi dan rantai pengawasan, mengurangi penipuan dan ketidakakuratan data. Kontrak pintar dapat mengotomatiskan pemeriksaan kepatuhan dan berintegrasi dengan model perkiraan AI untuk mengoptimalkan pasokan.
Q6: Apa aturan 30 menitnya?
Pedoman JPAC menyatakan bahwa unit RBC yang dikeluarkan dari penyimpanan bersuhu terkontrol harus dikembalikan ke dalam gudang 30 menit; jika mereka keluar 30–60 menit, mereka harus dikarantina selama enam jam sebelum diterbitkan kembali. Aturan tersebut mencegah siklus suhu berulang yang dapat merusak sel darah merah.
Ringkasan dan Rekomendasi
Menjaga integritas sel darah merah adalah tanggung jawab bersama para pendonor, bank darah, rumah sakit dan penyedia logistik. Poin-poin penting yang dapat diambil meliputi:
Patuhi rentang suhu: Simpan sel darah merah di 1–6 °C dan mengangkutnya ke 1–10 ° C.. Batasi kunjungan dan pantau terus menerus menggunakan sensor IoT.
Ikuti kerangka peraturan: Mematuhi FDA, UE, Pedoman PDB dan JPAC. Validasi peralatan, mengkalibrasi sensor dan mendokumentasikan setiap langkah.
Gunakan kemasan yang tervalidasi: Wadah prasyarat, meminimalkan ruang udara mati dan menggunakan PCM dan isolasi untuk menjaga suhu.
Latih staf dan rencanakan keadaan darurat: Pelatihan rutin memastikan tim Anda mengetahui cara menangani tamasya dan mengikuti aturan 30 menit. Mengembangkan rencana darurat untuk pemadaman listrik dan penundaan transportasi.
Rangkullah teknologi: Sensor IoT, drone, blockchain dan perkiraan AI dapat meningkatkan visibilitas, mengoptimalkan inventaris dan mendukung kepatuhan.
Langkah selanjutnya yang dapat ditindaklanjuti
Audit rantai dingin Anda: Lakukan penilaian komprehensif terhadap penyimpanan Anda, wadah pengangkutan dan sistem pemantauan. Identifikasi kesenjangan terkait suhu dan persyaratan dokumentasi yang dijelaskan di atas.
Menerapkan pemantauan waktu nyata: Lengkapi setiap unit atau kontainer RBC dengan pencatat data IoT yang mencatat suhu setiap beberapa menit dan terintegrasi dengan perangkat lunak inventaris.
Validasi solusi pengemasan baru: Uji PCM dan pengirim berinsulasi untuk memastikan mereka dapat bertahan 2–8 ° C. untuk durasi yang diperlukan, dan mendokumentasikan hasilnya.
Perbarui SOP: Merevisi prosedur operasi standar untuk mencerminkan 2025 peraturan, termasuk aturan 30 menit dan protokol kontinjensi.
Latih tim Anda: Jadwalkan sesi tentang manajemen suhu, dokumentasi dan teknologi baru. Mendorong staf untuk segera melaporkan penyimpangan.
Berinteraksi dengan para ahli: Konsultasikan dengan spesialis rantai dingin dan penasihat regulasi untuk terus mengikuti perkembangan persyaratan dan inovasi.
Tentang tempk
Tempk adalah penyedia terkemuka solusi pengemasan dan pemantauan rantai dingin yang disesuaikan dengan layanan kesehatan, biofarmasi dan logistik ilmu hayati. Perusahaan mendesain Pengirim berinsulasi bersertifikat ISTA yang mempertahankan 2–8 ° C. hingga 72 jam menggunakan bahan pengubah fasa yang dapat digunakan kembali dan sensor pintar. Sistem mereka mematuhi Pedoman Praktik Distribusi yang Baik dan FDA serta dikalibrasi dengan standar NIST dan UKAS. Platform pemantauan digital Tempk menyediakan data suhu waktu nyata dan jalur audit, memungkinkan pelanggan untuk memenuhi peraturan RBC rantai dingin yang ketat dengan percaya diri. Keberlanjutan adalah inti dari misi Tempk; mereka memprioritaskan bahan yang dapat didaur ulang dan desain yang hemat energi.
Panggilan Tindakan
Jika Anda siap menjaga suplai darah Anda dan menyederhanakan kepatuhan, hubungi pakar Tempk untuk konsultasi yang dipersonalisasi mengenai pengoptimalan rantai dingin Anda. Tim mereka akan membantu Anda memilih solusi pengemasan, perangkat pemantauan dan sistem manajemen data yang memenuhi persyaratan peraturan, mengurangi limbah dan melindungi pasien.