Vaccine Cold Chain Guide 2025 – How to Protect Vaccines
Vaccines are fragile biological products that lose potency when exposed to heat, freezing or light. Itu Rantai dingin vaksin is the system of temperature controlled storage and transport that protects these products from manufacturer to point of use. As immunization campaigns expand and novel vaccines require ultra cold temperatures, managing the vaccine cold chain in 2025 has become even more complex. This guide explains why you should care about the vaccine cold chain, how to build a resilient system, and what trends are shaping its future.
Why do you need a vaccine cold chain? A look at the risks to vaccine effectiveness and patient safety and how temperature controls mitigate them.
How can you build an effective vaccine cold chain? Step by step guidance on equipment, kemasan, monitoring and training.
What challenges will you face in 2025? Insights into weather disruptions, last mile delivery and regulatory compliance.
Which innovations are reshaping cold chain logistics? Emerging technologies such as IoT sensors, AI driven analytics and renewable energy solutions.
Pertanyaan yang sering diajukan: Practical answers to common concerns about storage, transport and handling of vaccines.
Why is the Vaccine Cold Chain Important for Immunization Programs in 2025?
The vaccine cold chain maintains vaccine potency and protects public health. Vaccines and other biologics must stay within strict temperature ranges to remain effective. Misalnya, most vaccines need to be stored between 2 °C dan 8 ° C. (36 °F–46 °F). Some biologics require –50 °C to –15 °C, while ultra cold products need –90 °C to –60 °C. When temperatures stray outside these ranges, vaccines can lose potency, leading to ineffective immunization or adverse reactions.
Safeguarding Patient Health and Reducing Waste
Maintaining the vaccine cold chain protects patient health in three main ways:
Preserves vaccine efficacy: Temperature excursions can destroy the active ingredients in vaccines, making them ineffective. According to pharmaceutical guidelines, most standard vaccines lose potency when stored outside the 2 °C–8 °C range.
Minimizes wastage: Spoiled vaccines must be discarded. By preventing temperature breaches, pharmacies and health facilities reduce costly waste and avoid revaccination of patients.
Ensures compliance: Regulatory agencies like the CDC require providers to keep detailed temperature logs and use calibrated data loggers to monitor storage units. Maintaining a robust vaccine cold chain helps you meet these requirements and avoid penalties.
Real World Impact
A specialty pharmacy recently installed digital data loggers with remote alerts. During a heatwave, a refrigerator reached 9 ° C.; staff received an alarm and moved vaccines to a backup unit within minutes. Continuous monitoring saved over $50,000 in biologics and ensured patients stayed on schedule. Without a strong vaccine cold chain, these life saving medicines could have been lost.
How Can You Build an Effective Vaccine Cold Chain in 2025?
A robust vaccine cold chain involves equipment, kemasan, monitoring and trained personnel working together. The following steps help you build a system tailored to your needs while meeting 2025 peraturan.
1. Select the Right Equipment
Vaccines require dedicated refrigeration and freezer units. Household refrigerators often fluctuate and may not meet pharmaceutical standards. Choose medical grade refrigerators that maintain 2 °C–8 °C with minimal variation. For frozen vaccines or biologics that need –50 °C to –15 °C, invest in reliable freezers designed for medical use. Ultra cold vaccines, like mRNA or gene therapies, require specialized freezers capable of –90 °C to –60 °C.
Tip praktis: Pre condition your refrigeration units. Pre cool freezers and refrigerators to the required temperature before loading vaccines. Always allow space around containers for air circulation to prevent warm or cold pockets.
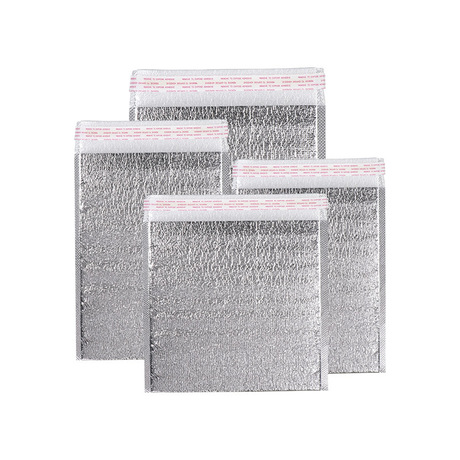
2. Use Insulated Packaging and Phase Change Materials
Packaging protects vaccines during transit. Insulated containers with phase change materials (PCMS) maintain stable temperatures for extended periods. Choose packaging rated for the specific temperature range and duration of your shipments. Validate your packaging under real world conditions to account for seasonal extremes.
Contoh: A community clinic uses insulated cartons lined with PCM packs that maintain a constant 5 ° C untuk 48 jam. Even in summer heat, vaccines arrive within the safe range, reducing waste and improving patient care.
3. Implement Continuous Temperature Monitoring
Digital data loggers (DDLs) and Internet of Things (IoT) sensors are the backbone of cold chain monitoring. They record temperatures at regular intervals and send alerts when readings go out of range. To comply with CDC guidelines, use calibrated loggers with buffered probes and keep calibration certificates up to date.
Tip praktis: Ensure each storage and transport container has its own data logger. Set alert thresholds slightly inside the acceptable range—for example, 3 °C dan 7 °C for a 2 °C–8 °C fridge—to allow time for corrective action.
4. Train Staff and Document Procedures
Human error is a common cause of vaccine cold chain failures. Develop standard operating procedures (Sops) covering temperature monitoring, emergency response and equipment maintenance. Train all staff to handle vaccines properly, record temperatures and respond to excursions. Maintain logs for every batch of vaccines and keep training records to satisfy regulatory audits.
5. Plan for the Last Mile and Emergencies
The final stage of vaccine delivery—the last mile—is prone to temperature excursions. Use validated shipping containers that maintain temperature beyond the delivery window. Consider using signature confirmation or smart lockers to reduce the time vaccines spend outside controlled environments. Always have backup power, extra ice packs and emergency transport containers to handle equipment failures or power outages.
Key Components of Vaccine Cold Chain Management
Your vaccine cold chain consists of several components that work together to ensure reliability. Understanding each helps you design a comprehensive system.
Storage Equipment
Refrigerators and freezers: The backbone of your vaccine cold chain. Ensure units are dedicated to vaccine storage to prevent temperature fluctuations. Separate refrigerators for vaccines and other medical products to avoid frequent door openings. For ultra cold storage, use specialized freezers and cryogenic units.
Perangkat pemantauan: Digital data loggers, IoT sensors and cloud based dashboards provide continuous temperature tracking. The ability to view real time data and receive alerts helps you respond quickly to excursions.
Bahan pengemasan
Wadah terisolasi: Cardboard boxes with foam insulation, vacuum insulated panels or expanded polystyrene (EPS) protect vaccines from external temperature changes. Choose materials based on the required duration and temperature range.
Bahan perubahan fase (PCMS): Substances that absorb or release heat as they change phase, such as water based gels or eutectic plates. PCMs maintain specific temperature ranges longer than ice or gel packs, reducing the risk of freezing or overheating.
Temperature logs and certificates: Regulatory agencies require documentation of temperature readings for vaccines. Keep calibration certificates for all monitoring devices and maintain logs of equipment maintenance.
Prosedur operasi standar (Sops): Provide clear instructions for receiving, menyimpan, transporting and handling vaccines. Include emergency response plans for temperature excursions, power failures and natural disasters.
Pelatihan Staf
Ongoing education: Regular training ensures staff understand how to load refrigerators, check temperature logs and handle vaccines quickly. Conduct drills on emergency procedures and validate competency through observation or assessments.
Practical Storage & Transport Tips
| Skenario | Tip | Mengapa itu penting |
| Receiving shipments | Inspect packaging, verify indicators, and record arrival temperature immediately | Early detection of temperature excursions prevents compromised vaccines from entering inventory |
| Penyimpanan | Keep vaccines in dedicated refrigerators or freezers; avoid overstocking to maintain airflow | Adequate airflow prevents hot or cold spots that damage vaccines |
| Pengeluaran | Minimize time outside refrigeration; use insulated containers for transport | Preserves vaccine potency when moving from storage to patients |
| Wadah pra-kondisi | Pre cool refrigerators and insulated containers before loading vaccines | Prevents temperature spikes during loading |
| Labeling and educating patients | Clearly mark packages with required temperature range and instruct patients to refrigerate immediately | Ensures proper handling during last mile and at home |
Useful Tips for Different Scenarios
Clinic with multiple storage units: Assign each refrigerator and freezer its own data logger and daily checklist. Set up a weekly rotation for staff to cross audit logs, which helps catch errors early.
Transport to remote vaccination sites: Use portable vaccine carriers with PCM packs rated for 2 °C–8 °C. Include a backup PCM pack in case of delays. For vaccines requiring –20 °C, carry an extra dry ice container and a digital thermometer.
Home health programs: Send patients home with insulated bags and clear instructions to refrigerate vaccines immediately. Provide a simple thermometer for patients to verify their fridge stays between 2 °C dan 8 ° C..
Contoh dunia nyata: A community pharmacy replaced household refrigerators with medical grade units and implemented continuous monitoring. By labeling packages and clearly communicating storage requirements, they reduced spoilage by 20 % and passed regulatory inspections.
Overcoming Challenges in Vaccine Cold Chain: Weather, Last Mile and Compliance
Environmental and operational challenges can disrupt your vaccine cold chain. Weather extremes, infrastructure limitations and regulatory changes make 2025 particularly challenging. Understanding these risks helps you plan ahead.
Weather and Climate Risks
Heatwaves, cold snaps, storms and floods can cause power outages and disrupt transportation. During extreme weather, your storage units may struggle to maintain temperatures. Prepare by installing backup power generators, battery powered refrigerators and surge protectors. Use predictive weather data to schedule deliveries during favorable conditions.
Pengiriman Mile Terakhir
The last mile is the portion from the final distribution center to the vaccination site. Temperature excursions often occur during this stage due to delays, improper handling or inadequate packaging. Mitigate risks by:
Using insulated shippers validated to maintain temperature beyond the expected transit time.
Tracking shipments in real time with GPS and temperature sensors.
Training couriers and volunteers on proper handling and the importance of timely delivery.
Coordinating with clinics to ensure someone is available to receive and store vaccines immediately.
Regulatory Compliance and Documentation
Regulators continually update standards for vaccine storage and handling. Di dalam 2025, expect stricter monitoring requirements, including digital logging and real time reporting. Stay compliant by:
Keeping calibration certificates for every data logger.
Documenting daily temperature readings and corrective actions.
Conducting internal audits and readiness assessments before inspections.
Maintaining training records to demonstrate staff competency.
Human Factors and Training
Staff turnover, fatigue and misunderstanding can cause errors such as leaving refrigerators open or misreading thermometers. Mitigate by standardizing procedures, conducting regular training and using checklists. Encourage a culture of accountability and empower staff to report issues without fear of punishment.
Infrastructure and Resource Constraints
In remote or low resource settings, infrastructure may be limited. Solar powered refrigerators and portable vaccine carriers can help maintain the vaccine cold chain without grid electricity. Partnerships with logistics providers for last mile delivery—such as drones or motorcycles—can overcome transportation challenges in rural areas.
Vaccine Cold Chain Innovations and Trends in 2025
Emerging technologies are transforming the vaccine cold chain. As demand for biologics grows and supply chains become more complex, innovations help maintain quality, reduce costs and improve sustainability.
Internet of Things (IoT) and Real Time Monitoring
IoT sensors embedded in storage units and packaging send real time temperature data to cloud platforms. These systems provide alerts when temperatures drift and allow remote troubleshooting. Integration with GPS enables location and condition tracking throughout transit. This transparency reduces the risk of unnoticed excursions.
Kecerdasan Buatan dan Analisis Prediktif
AI algorithms analyze historical temperature data, weather forecasts and shipment schedules to predict potential disruptions. By anticipating delays or equipment failures, logistics planners can reroute shipments or allocate backup equipment proactively. AI also optimizes routing to reduce transit time and energy use.
Blockchain untuk Ketertelusuran
Blockchain technology creates immutable records of vaccine temperature data, custody and location. This improves trust and accountability across the supply chain. Di dalam 2025, some national immunization programs are piloting blockchain systems to authenticate vaccine batches and monitor their journey from manufacturer to patient.
Renewable Energy Solutions
To address energy reliability and sustainability, innovators are developing solar powered vaccine refrigerators, wind powered monitoring systems and hydrogen fuel cells for portable units. These solutions reduce dependency on grid electricity and align with global sustainability goals.
Autonomous Delivery Vehicles
Drones and self driving vehicles are increasingly used for last mile delivery in hard to reach areas. They can carry small vaccine payloads while maintaining temperature control. When combined with real time monitoring, these vehicles ensure vaccines arrive quickly and safely.
Kemasan Berkelanjutan
Kotak terisolasi yang dapat digunakan kembali, biodegradable phase change materials and recyclable cushioning reduce waste and carbon footprint. Di dalam 2025, many health organizations are adopting reusable vaccine carriers that can be sanitized and redeployed, cutting costs and environmental impact.
Market and Regulatory Insights for 2025
Demand for vaccine cold chain solutions is growing. Global immunization programs are expanding, and new biologics require cold or ultra cold storage. Analysts project the cold chain logistics market to reach hundreds of billions of dollars by the early 2030s. Governments and health organizations are increasing investments in infrastructure, training and technology.
Regulatory agencies are tightening standards for vaccine storage and transport. Expect mandatory digital temperature monitoring, enhanced reporting and greater accountability. Financial penalties for improper storage or spoiled vaccines will rise. Businesses should stay ahead of these changes by adopting robust monitoring and documentation systems.
Pertanyaan yang sering diajukan
Q1: What temperature range is required for standard vaccines?
Standard vaccines should be stored between 2 °C dan 8 ° C. (36 °F–46 °F). Deviating from this range can lead to potency loss. Always use dedicated medical refrigerators and monitor temperatures continuously.
Q2: How long can vaccines remain outside refrigeration during a clinic session?
Limit the time vaccines spend at room temperature to a minimum. Idealnya, vaccines should not remain unrefrigerated for more than 30 menit. Use insulated carriers and quickly return unused doses to the refrigerator.
Q3: What should I do if my data logger shows a temperature excursion?
Immediately quarantine the affected vaccines. Record the duration and temperature of the excursion, and consult the vaccine manufacturer’s guidelines to determine if the product remains usable. Document the incident and implement corrective actions.
Q4: Are household refrigerators acceptable for vaccine storage?
Household refrigerators are not recommended because they experience significant temperature fluctuations. Use medical grade units designed specifically for vaccines and maintain them according to manufacturer instructions.
Q5: How do I train staff on vaccine cold chain procedures?
Create comprehensive SOPs covering receiving, penyimpanan, transport and emergency response. Conduct regular training sessions, hands on demonstrations and drills. Maintain records of training to demonstrate compliance during inspections.
Q6: What innovations should I consider adopting in 2025?
Look into IoT monitoring, Pengoptimalan rute yang digerakkan oleh AI, blockchain traceability and renewable energy sources. These technologies enhance visibility, reduce costs and support sustainability goals.
Ringkasan dan Langkah Selanjutnya
Summary of key points: Maintaining an effective vaccine cold chain ensures vaccine potency, reduces waste and meets regulatory requirements. Equip yourself with medical grade refrigeration and insulated packaging. Implement continuous monitoring using calibrated data loggers and IoT sensors. Train staff thoroughly and document every step. Plan for last mile delivery and emergencies. Stay informed about innovations such as IoT, Ai, blockchain and renewable energy to enhance resilience. When temperatures are strictly controlled, vaccines remain safe and effective.
Langkah selanjutnya yang dapat ditindaklanjuti:
Assess your current vaccine cold chain equipment and replace any household refrigerators with medical grade units.
Implement digital data loggers in every storage and transport unit and set up remote alerts.
Review your SOPs and update them to reflect the latest guidelines. Train your team on these procedures and record their training.
Pilot at least one innovative technology—such as an IoT monitoring platform or solar powered refrigerator—to improve resilience and sustainability.
Regularly audit your vaccine cold chain and make adjustments based on data and feedback. Seek expert advice from cold chain specialists when needed.
Tentang tempk
Kami adalah Tempk, a global leader in temperature controlled packaging and cold chain solutions. Our mission is to help healthcare providers and pharmaceutical companies protect the integrity of vaccines, biologics and other sensitive products. We design and manufacture insulated containers, phase change materials and monitoring devices that meet stringent regulatory standards. By combining innovative technology with deep industry expertise, we provide reliable, sustainable and cost effective cold chain solutions tailored to your needs.
Panggilan untuk bertindak: Siap memperkuat rantai dingin vaksin Anda? Contact us for personalized consultation and discover how our solutions can protect your vaccines in 2025 dan seterusnya.