Sistem Rantai Dingin Vaksin: Bagaimana cara kerjanya & Mengapa itu penting?
Itu vaccine cold chain system is the foundation of modern immunization programmes. It is the network of people, equipment and procedures that keep vaccines within safe temperature limits from manufacturing to injection. Without a robust vaccine cold chain system, vaccines quickly lose potency – studies show that vaccines exposed to temperatures above 8 °C can lose up to 20 % of their effectiveness in just one hour. This guide explains how the vaccine cold chain system works, the recommended temperature ranges, monitoring technology and emerging trends so you can protect every dose.

What the vaccine cold chain system is and why it matters – including the key elements (personnel, equipment and procedures).
Safe temperature ranges for vaccines and their categories – refrigerated, frozen and ultra cold vaccines and the consequences of temperature excursions.
Critical equipment for storage and transport – refrigerators, freezer, digital data loggers and insulated containers.
Best practices for monitoring and standard operating procedures – how to use digital data loggers, record temperatures and train staff..
Transportation methods and packaging choices – gel packs, es kering, liquid nitrogen and IoT enabled logistics.
Inovasi dan tren pasar untuk 2025 – blockchain, solar powered storage, AI route optimisation and the growth of the global vaccine cold chain logistics market.
What Is a Vaccine Cold Chain System and Why Is It Essential?
A vaccine cold chain system ensures that vaccines stay within their prescribed temperature range throughout their journey. It comprises trained personnel, purpose built equipment and standard operating procedures. Without these components working together, vaccines may be exposed to damaging heat or cold, leading to lost potency, wasted doses and outbreaks of preventable diseases. nyatanya, research suggests that as many as 35 % of vaccines are compromised because of temperature mishandling, resulting in costly revaccination campaigns and reduced public confidence.
Why Temperature Control Protects Potency
Vaccines are biological products. Heat can degrade proteins and fats; freezing can cause ice crystals that damage their structure. Most routine vaccines require refrigeration between 2 °C dan 8 ° C.. Live attenuated vaccines such as varicella and some COVID 19 formulations require freezing between –50 °C and –15 °C, ketika mRNA vaccines often need ultra cold storage between –90 °C and –60 °C. Paparan suhu di atas 8 °C for just one hour may reduce potency by 20 %. Sebaliknya, freezing aluminium containing vaccines causes clumping and irreversible damage. Maintaining the right range is therefore critical for efficacy.
Key Elements of the Vaccine Cold Chain System
Itu three key elements of the vaccine cold chain system are personnel, equipment and procedures:
Personnel – a trained vaccine and cold chain handler manages storage, monitors temperatures and maintains records. At each facility there should be a designated coordinator responsible for training staff, ordering inventory and implementing emergency plans.
Peralatan – purpose built refrigerators, freezer, ice lined refrigerators (ILRs), kotak dingin, data loggers and transport vehicles ensure vaccines remain in range. Equipment can be electrical (powered by mains or solar) or non electrical (ice packs and vaccine carriers).
Prosedur – standard operating procedures (Sops) outline how to load units, arrange vaccines by expiry date, record temperatures and respond to excursions. Without clear procedures, equipment and people cannot prevent temperature damage.
A strong vaccine cold chain system protects the potency of vaccines, reduces waste and builds public trust.
How the Vaccine Cold Chain System Works Across the Supply Chain
The vaccine cold chain system begins at the manufacturing plant and continues through national and local storage facilities to the clinic. At each link, temperatures must be maintained and documented. Menurut Organisasi Kesehatan Dunia, vaccines travel from the manufacturer to primary stores, district stores and clinics via refrigerated or insulated vehicles, cold boxes and vaccine carriers. These transport stages use controlled ranges such as +2 ° C ke +8 °C for refrigerated vaccines and –15 °C to –25 °C for frozen vaccines. Each store uses equipment like walk in coolers (WICs), walk in freezers (WIFs), ice lined refrigerators and deep freezers to keep doses safe.
Manufacturing – Vaccines are produced under strict conditions and immediately cooled. They are packaged in vials or syringes and placed in shipping containers with data loggers and refrigerants. Manufacturers must coordinate with logistics providers to prepare for specific temperature needs.
Primary and district storage – Walk in coolers and walk in freezers receive bulk shipments. Staff monitor temperatures at least twice daily and ensure stock rotation using the “first expiring, first out” method.
Angkutan – Insulated vans, refrigerated trucks or passive cold boxes move vaccines to regional or local facilities. Data loggers travel with shipments, recording temperatures at least every 30 menit.
Local storage and administration – Clinics use ice lined refrigerators or small freezers to store vaccines until administration. Vaccine carriers maintain the correct temperature during outreach sessions. Staff check min/max temperatures each workday and update logs.
By maintaining the cold chain from start to finish, the vaccine cold chain system ensures that each dose delivers its intended protection.
Safe Temperature Ranges and Vaccine Categories
Different vaccines require different storage conditions. Knowing the required temperature range for each vaccine type is essential for the vaccine cold chain system. The following categories summarise the main requirements:
| Vaccine Category | Kisaran suhu | Contoh Vaksin | Makna |
| Didinginkan | 2 °C – 8 ° C. (36 °F – 46 ° f) | Influensa, DTaP, HPV, MMR dan sebagian besar vaksin rutin | Kisaran paling umum. Maintaining around 5 °C reduces fluctuations. |
| Beku | –50 °C – –15 °C (–58 °F – 5 ° f) | Varisela, mpox (Jynneo) and some COVID 19 vaccines | Diperlukan untuk vaksin hidup yang dilemahkan; exposure to warmer temperatures compromises viral components. |
| Sangat dingin | –90 °C – –60 °C (–130 °F – –76 °F) | vaksin mRNA seperti Pfizer–BioNTech Comirnaty | Diperlukan untuk penyimpanan jangka panjang. Some vials can be thawed and stored at 2 °C–8 °C for up to ten weeks. |
Most vaccines used today fall into the refrigerated category and must never be frozen. Freezing aluminium adjuvanted vaccines causes clumping and irreversible damage. Sebaliknya, some formulations (MISALNYA., Vaksin mRNA) lose potency quickly if allowed to thaw and must be kept in ultra cold freezers or moved to refrigerated storage just before use.
Consequences of Temperature Excursions
Even brief deviations outside the prescribed range can have serious consequences. A one hour exposure above 8 °C can reduce vaccine effectiveness by up to 20 %. Frozen vaccines thawed accidentally must be discarded, and ultra cold vaccines that warm above –60 °C cannot be returned to storage. Because potency cannot be restored, the vaccine cold chain system prioritises prevention through accurate temperature control and monitoring.
Essential Equipment for the Vaccine Cold Chain System
Purpose built equipment is the backbone of the vaccine cold chain system. Household refrigerators are not adequate because they have wide temperature fluctuations and uneven cooling. The following equipment categories keep vaccines within range:
Pharmaceutical grade refrigerators and freezers – These units maintain stable temperatures within the recommended range and include features like alarms, lockable doors and shelves that allow airflow. Ice lined refrigerators (ILRs) store vaccines at +2 ° C ke +8 °C and have a holdover time of 20 jam di 43 ° C., meaning they maintain temperature during power cuts. Deep freezers maintain –15 °C to –25 °C and store ice packs or vaccines requiring freezing.
Ultra cold freezers – Designed for mRNA vaccines, these units maintain –90 °C to –60 °C. They often require backup power and have smaller capacity due to insulation thickness.
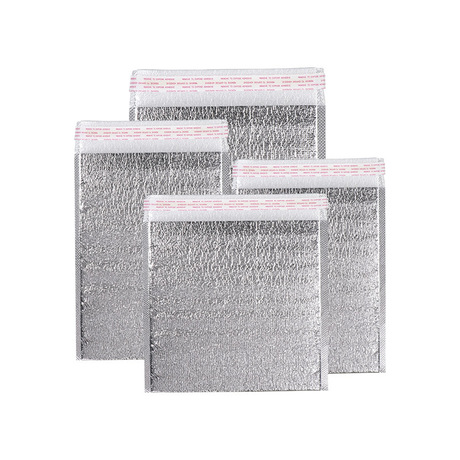
Cold boxes and vaccine carriers – Passive containers lined with insulation and filled with conditioned ice packs or phase change materials (PCMS). They are used for transport or outreach sessions and can maintain +2 ° C ke +8 °C hingga 96 hours in hot conditions.
Insulated vans and refrigerated vehicles – Vehicles equipped with refrigeration units to transport vaccines between hubs. They are used for both refrigerated (+2 ° C ke +8 ° C.) dan beku (–15 °C to –25 °C) produk.
Solar powered refrigerators – Ideal for remote areas without reliable electricity. They use solar panels and batteries to maintain vaccine temperatures. Solar cold storage reduces energy costs; commercial electricity averaged 13.10 cents per kilowatt hour in 2024, sedangkan tarif tenaga surya berkisar antara 3.2 ke 15.5 sen per kWh.
Avoiding Inadequate Equipment
Use of combination household refrigerators or dorm style fridges is discouraged. They often experience temperature fluctuations and have freezer compartments that can accidentally freeze vaccines. When pharmaceutical grade units are unavailable, a standalone refrigerator may be used temporarily but requires careful monitoring. Always place vaccines in their original boxes away from walls and doors, and never store food or beverages in the same unit.
Monitoring Temperature: Digital Data Loggers and Best Practices
Continuous temperature monitoring is the heart of the vaccine cold chain system. AS. Pusat Pengendalian dan Pencegahan Penyakit (CDC) recommends using digital data loggers (DDL), which record temperatures at preset intervals and provide detailed histories. Unlike simple thermometers, DDLs capture trends and alert staff before vaccines are compromised.
Features of an Effective Digital Data Logger
A reliable DDL should include:
| Fitur | Mengapa itu penting | Keuntungan |
| Pemeriksaan yang disangga | Mengukur suhu cairan, bukan udara, mimicking vaccine conditions | Prevents false alarms when doors open and reduces unnecessary transfers |
| Alarm di luar jangkauan | Memberi tahu staf segera ketika suhu menyimpang | Enables rapid corrective action, menghemat vaksin |
| Interval pencatatan yang dapat diprogram | Memungkinkan perekaman setidaknya setiap 30 menit | Memberikan riwayat suhu terperinci untuk audit |
| Calibration and accuracy | Uncertainty of ±0.5 °C and periodic calibration ensure reliable readings | Ensures compliance and protects vaccine potency |
| Cloud connectivity and remote access | Sends real time data and alerts to remote devices | Enhances oversight and facilitates rapid response |
The CDC recommends that every storage and transport unit have a DDL and that at least one backup device be available. Staff should download and review DDL data at least every two weeks and keep records for three years. Calibration certificates should indicate the model, serial number, date of calibration, and uncertainty.
Standard Operating Procedures and Training
Monitoring alone is insufficient without clear procedures and trained staff. Each facility should develop standard operating procedures covering storage, penanganan, pemantauan, tanggap darurat dan dokumentasi. Key practices include:
Recording minimum and maximum temperatures at the start of each workday; if DDLs display min/max readings, staff still record them daily.
Training all personnel who handle vaccines, with orientation and annual refresher courses. Scenario based drills prepare teams for power outages, equipment failure and natural disasters.
Creating an emergency plan outlining backup power sources, alternative storage locations and contact information.
Document retention – maintain temperature logs and calibration certificates for at least three years.
A robust SOP ensures that the vaccine cold chain system functions smoothly even during unexpected events.
Transport and Packaging: Protecting Vaccines on the Move
Maintaining temperatures during transport is just as important as during storage. The vaccine cold chain system uses various packaging methods and refrigerants depending on the required temperature range. Menurut riset pasar, the global vaccine cold chain logistics market was valued at USD 3.5 miliar masuk 2024 and is predicted to reach USD 5.9 miliar oleh 2034 dengan CAGR sebesar 5.3 %. Growth is driven by increased vaccine production, advances in packaging technologies and growing awareness of health and wellness.
Packaging Methods and Refrigerants
Es kering (karbon dioksida padat) – provides temperatures around –78 °C and is suited for frozen or ultra cold shipments. It sublimates rather than melts, but shipping regulations limit the amount that can be used.
Paket gel dan bahan pengubah fasa (PCMS) – maintain 2 °C–8 °C untuk vaksin yang didinginkan. PCMs absorb or release heat at specific temperatures, extending hold times.
Nitrogen cair – enables cryogenic conditions below –150 °C for cell and gene therapies.
Use validated containers and pack out designs that match the expected ambient conditions and transit time. Always include a calibrated DDL inside shipments and select shipping routes that minimize transit time and handling.
IoT Enabled Sensors and AI Driven Logistics
Logistik rantai dingin modern semakin diandalkan smart sensors that transmit real time temperature, data kelembaban dan lokasi. Saat sensor mendeteksi suhu yang tidak aman, they automatically alert users via text, email or mobile app. Integrating sensors with GPS provides visibility across the supply chain and allows rapid intervention. Kecerdasan buatan (Ai) algorithms analyze traffic and weather data to optimise routes and reduce transit time. Predictive analytics identify patterns and trigger alerts before excursions occur, making the vaccine cold chain system more resilient.
Innovations Shaping the Vaccine Cold Chain System in 2025
The vaccine cold chain system is evolving rapidly. Technologies emerging in 2025 meningkatkan transparansi, keberlanjutan dan efisiensi, helping to meet the growing demand for vaccines and comply with stricter regulations. highlights several key innovations:
Blockchain untuk ketertelusuran ujung ke ujung – Distributed ledger technology records every transaction in the supply chain, membuat log suhu anti rusak, location and handover events. This transparency facilitates audits and reduces the risk of data manipulation.
Penyimpanan dingin bertenaga surya – Off grid solar units provide reliable refrigeration in areas with unstable electricity. Solar cold storage reduces operational costs; di dalam 2024 commercial electricity averaged 13.10 ¢/kWh while solar rates ranged from 3.2 ke 15.5 ¢/kWh.
Sensor cerdas yang mendukung IoT – Wireless sensors deliver real time data and alerts, reducing operational risk. Coupled with GPS, mereka memungkinkan visibilitas lengkap dari asal ke tujuan.
Pengoptimalan rute bertenaga AI – AI analyses traffic and weather patterns to choose routes that maintain temperature stability and reduce transit time.
Freezer kriogenik portabel – Compact units maintain –80 °C to –150 °C, enabling safe transport of cell and gene therapies and ultra cold vaccines.
Kemasan berkelanjutan – Recyclable containers, biodegradable thermal wraps and reusable cold packs reduce environmental impact while maintaining temperature.
These innovations not only enhance performance but also align the vaccine cold chain system with corporate environmental, sosial dan pemerintahan (ESG) commitments.
Market Insights and Growth Drivers
Sektor rantai dingin mendukung industri makanan dan farmasi, but vaccines represent a high stakes segment. The global cold chain market is expected to grow from USD 418.81 miliar masuk 2025 ke USD 1,416.67 miliar oleh 2034, mewakili a 14.5 % tingkat pertumbuhan tahunan gabungan (CAGR). Amerika Utara bertahan 36 % pendapatan dan terus berinvestasi pada teknologi hemat energi. Pada saat yang sama, the dedicated vaccine cold chain logistics market will expand from USD 3.5 miliar masuk 2024 ke USD 5.9 miliar oleh 2034.
Drivers of growth include:
Melonjaknya produksi vaksin – The ongoing rollout of mRNA boosters and cell therapies necessitates more cold chain capacity.
Inovasi teknologi – IoT sensors, blockchain dan AI meningkatkan efisiensi dan mengurangi pemborosan.
Memperluas akses layanan kesehatan – Rural immunisation programmes and global disease eradication initiatives require reliable cold storage in remote areas.
Kepatuhan Pengaturan – Stricter guidelines for temperature monitoring, dokumentasi dan keamanan memaksa fasilitas untuk meningkatkan peralatan dan sistem.
Fokus pada keberlanjutan – Governments and companies prioritise renewable energy and recyclable materials in cold chain operations.
Understanding these trends helps organisations anticipate future needs and plan investments accordingly.
2025 Perkembangan dan Tren Terkini
2025 brings new developments that reshape the vaccine cold chain system:
Connected cold chains become the norm – Integration of IoT sensors, AI and blockchain fosters end to end visibility and proactive intervention. Facilities can monitor shipments in real time and quickly respond to excursions.
Stricter compliance and auditing – Regulatory bodies such as the CDC, WHO and EU GDP require continuous temperature monitoring, pencatatan rinci dan kalibrasi teratur.
Rising demand for ultra cold storage – The popularity of mRNA boosters and biologics drives investment in cryogenic freezers and specialized packaging.
Sustainability integration – Companies adopt solar powered units and recyclable packaging to reduce energy consumption and waste.
Rantai pasokan vaksin digital (DVSC) – Modern information technology tracks and manages vaccine processes in real time, meningkatkan transparansi dan efisiensi. The World Health Organization’s Global Strategy on Digital Health (2020–2025) encourages countries to leverage digital technologies to improve vaccine supply chain management.
By embracing these trends, organisations can future proof their vaccine cold chain systems.
Pertanyaan yang sering diajukan
Q1: Berapa lama vaksin mRNA dapat disimpan pada suhu lemari es?
Setelah pencairan, some mRNA vaccines such as Pfizer–BioNTech Comirnaty may be kept at 2 °C–8 °C for up to ten weeks. Always refer to the manufacturer’s product insert and monitor temperatures continuously.
Q2: Apa yang harus saya lakukan jika vaksin terkena suhu di atas 8 ° C.?
Perubahan suhu apa pun dapat menurunkan potensi. Immediately quarantine the affected vaccines, beri label “jangan gunakan,” and contact the manufacturer or immunisation programme for guidance. Studies show that a one hour exposure above 8 °C may reduce vaccine effectiveness by up to 20 %. Never administer compromised doses.
Q3: Bisakah saya menggunakan lemari es rumah tangga untuk menyimpan vaksin?
Household refrigerators may be used only if pharmaceutical grade units are unavailable. Combination units and dorm style fridges are not acceptable; they have uneven temperatures and can freeze vaccines. If a household refrigerator is used, place vaccines in the centre, away from walls and the door, and monitor temperatures closely.
Q4: Seberapa sering saya harus mencatat suhu?
CDC merekomendasikan untuk memeriksa dan mendokumentasikan suhu minimum dan maksimum setidaknya dua kali sehari dan mengunduh data dari logger digital setiap dua minggu atau setelah perjalanan apa pun. Jika logger Anda menampilkan pembacaan min/maks, mencatatnya pada awal setiap hari kerja.
Q5: Apa saja yang harus disertakan dalam rencana rantai dingin darurat??
A robust plan should cover backup power sources, lokasi penyimpanan alternatif, kontainer transportasi dan informasi kontak darurat. Lakukan latihan rutin dan pastikan semua staf mengetahui langkah-langkah untuk mentransfer vaksin dengan aman selama pemadaman listrik atau kegagalan peralatan.
Ringkasan dan Rekomendasi
Di dalam 2025 the vaccine cold chain system is more critical than ever. Keeping vaccines potent requires strict adherence to temperature ranges (2 °C–8 °C for most vaccines, –50 °C– –15 °C for live attenuated vaccines and –90 °C– –60 °C for mRNA formulations). Use pharmaceutical grade refrigerators, freezers and ultra cold units; avoid household combination refrigerators and overcrowding. Melaksanakan calibrated digital data loggers with buffered probes, alarms and cloud connectivity to monitor temperatures continuously. Develop standard operating procedures, train staff regularly, and prepare for emergencies. Merangkul inovasi seperti sensor IoT, Pengoptimalan rute AI, ketertelusuran blockchain dan penyimpanan bertenaga surya to enhance efficiency and sustainability. Akhirnya, tetap mendapat informasi tentang tren pasar, regulatory changes and new technologies to future proof your vaccine cold chain system.
Rencana aksi: Next Steps for Optimising Your Vaccine Cold Chain System
Audit your equipment – Assess your current refrigerators, freezers and data loggers. Replace any combination or dorm style units with pharmaceutical grade models. Verify calibration certificates and plan replacements for units approaching the end of their service life.
Implement or upgrade digital monitoring – Invest in high precision digital data loggers with glycol buffered probes, out of range alarms and cloud connectivity. Ensure the logging interval is at least every 30 minutes and keep backup devices.
Develop comprehensive SOPs and training programmes – Create written procedures covering storage, mengangkut, pemantauan dan tanggap darurat. Train all staff upon hire and provide annual refresher courses. Conduct regular drills to test the emergency plan.
Explore innovations and sustainability – Evaluate the feasibility of solar powered refrigerators for off grid sites and Sensor IoT untuk pemantauan waktu nyata. Consider sustainable packaging options like reusable containers and biodegradable thermal wraps.
Monitor market and regulatory updates – Stay informed about evolving guidelines from the CDC, WHO and national authorities. Monitor market trends such as the growth of the vaccine cold chain logistics market and emerging technologies.
By following this action plan you can strengthen your vaccine cold chain system, reduce waste and ensure that every dose administered delivers full immunity.
Tentang tempk
Tempk is a leading innovator in cold chain solutions for healthcare and life sciences. We design and manufacture pharmaceutical grade refrigerators, freezer, insulated containers and state of the art temperature monitoring systems. Our products feature advanced insulation, digital data loggers with cloud connectivity and options for solar power integration, enabling reliable storage in remote locations. We are committed to sustainability and offer reusable packaging and biodegradable thermal wraps to reduce environmental impact. Dengan R yang berdedikasi&D team and strict quality standards, we help you safeguard vaccines and support regulatory compliance.
Ready to optimise your vaccine cold chain system? Hubungi spesialis kami today for a customised assessment and discover how Tempk can help you maintain potency, reduce waste and embrace the innovations of 2025.