Medical Ice Box Provider: How Do You Choose in 2026?
Last updated: January 8, 2026
Choosing the right medical ice box provider is not just a packaging decision. It’s a patient-safety and audit-risk decision. If you ship 2–8°C vaccines, biologics, or lab samples, even a short drift can turn usable products into waste. Many lanes need 48–96 hours of protection once you include real delays, not perfect schedules. In this guide, you’ll learn how to pick a medical ice box provider using lane fit, proof documents, and simple pack-out execution.
This article will help you:
Shortlist a medical ice box provider for 2–8°C shipping using a lane-risk self-test
Request temperature validation reports that match your real routes and handling
Reduce freeze risk with pack-out rules and physical separators
Compare reusable vs. single-use systems with practical ROI signals
Build a GDP-ready vendor checklist that makes audits less stressful
What does a medical ice box provider actually deliver?
A medical ice box provider should deliver a controlled shipping system, not only an insulated box. That system includes the container, the coolant plan, the pack-out steps, and the proof that the configuration works under defined conditions. If a provider only sells “a box,” you will end up patching the system later with guesswork and rushed packing.
In plain terms, think of it like a seatbelt. The belt matters, but so do the anchor points and the crash test. Your medical ice box provider should give you the “crash test” for temperature: clear assumptions, clear results, and a pack-out your team can repeat without hero-level skill.
The 5 non-negotiables from a validated medical ice box provider
A validated medical ice box provider should be able to hand you five items quickly, without confusion. If any item is missing, your operational risk rises.
| What you need | What to ask for | What it means for you |
| Thermal performance proof | “Show me the temperature curve and test conditions.” | You stop buying “hours” and start buying evidence |
| Pack-out SOP (visual) | “Do you have a photo-based packing guide?” | Faster training, fewer packing errors |
| Configuration clarity | “Which coolant plan fits my lane time?” | Less overpacking, fewer surprises |
| Change control | “How do you notify material or design changes?” | No silent performance drift |
| Supply stability | “What’s your real capacity and lead time?” | Fewer stockouts during peak demand |
Practical tips you can use today
Ask for your “worst day” design target: hot weather + late pickup + missed delivery attempt.
Reject vague language: if you hear “usually” or “around,” ask for test assumptions.
Demand “sample equals production”: your pilot unit must match mass production.
Example scenario: One clinic program reduced loss after switching to a medical ice box provider that validated temperature recovery after repeated lid openings.
How do you match a medical ice box provider to your lane risk?
The best medical ice box provider is the one that fits your lane behavior, not your product name. Two vaccine shipments can be completely different if one stays local and the other crosses hubs. Start by mapping time, handoffs, and exposure—then add a delay buffer that reflects reality.
A good medical ice box provider will ask you lane questions first: transit time, dwell time, delivery windows, weekend risk, and how often boxes get opened. If they do not ask, you may be buying a box that only works in a lab-perfect world.
Lane-risk self-test (2 minutes)
Score each item 0–2. Total is 0–12.
Do you ship during peak heat or cold seasons?
Do shipments sit in a hub or warehouse over 6 hours?
Do you face missed delivery attempts or appointment delays?
Do you ship to rural or hard-to-reach facilities?
Do you ship with weekend or holiday risk?
Do you rely on pickup windows you cannot control?
How to read your score
9–12 (High risk): You need lane-specific configurations and larger buffer time.
5–8 (Medium risk): You need optimized coolant plus clear SOP discipline.
0–4 (Lower risk): You can optimize cost, but you still need proof.
Matching lane risk to packaging strategy
| Lane risk | Typical protection goal | Typical approach | What it means for you |
| Low | Transit time + 8–12h buffer | Standard gel/PCM plan | Efficient cost and speed |
| Medium | Transit time + 12–24h buffer | Strong insulation + tuned coolant | Fewer “surprise” drifts |
| High | Transit time + 24–48h buffer | Higher-grade insulation + modular coolant | Better outcomes during chaos |
Practical tips you can use today
Evaluate on your hardest lane first. If it passes there, others are easier.
Get buffer time in writing. A medical ice box provider should state the design target.
Keep pack-out simple. Complexity is a hidden failure driver.
What proof should a medical ice box provider show before you buy?
A medical ice box provider should prove performance with readable validation, not marketing claims. You want test assumptions, pack-out diagrams, and revision control. If evidence is missing, the “savings” often reappear later as re-ships, waste, and customer complaints.
Proof should be simple enough that you can explain it to operations, quality, and procurement in one meeting. If the provider’s report cannot be explained in plain language, defending it during an audit becomes harder.
Validation evidence that matters in real operations
| Evidence | What it proves | Red flags | What you should do |
| Thermal profile report | Temp vs time under defined conditions | Missing ambient range or payload | Request full conditions and duration |
| Pack-out sheet / SOP | Coolant placement and steps | No photos, unclear steps | Require a visual SOP |
| Spec sheet | Materials, dimensions, tolerances | “Equivalent material” wording | Ask for exact BOM and tolerances |
| Batch inspection record | Consistency across production | No batch IDs | Require batch traceability |
| Change notification | Controls when parts change | No written policy | Put notice rules in purchase terms |
The “5-item proof checklist” (print this)
Before you approve a medical ice box provider, confirm you have:
A configuration-specific thermal report (not generic)
A photo SOP with common mistakes listed
A spec sheet with material names and tolerances
A written change-control statement with notice timing
A re-validation trigger plan when design or materials change
Practical tips you can use today
Ask for coolant start temperatures. They can change outcomes more than people expect.
Confirm payload mass in testing. Light payloads can warm faster than heavy payloads.
Demand “conditions + curve,” not “pass/fail.” Curves reveal hidden risk.
How do you avoid freezing risk in 2–8°C shipping?
A strong medical ice box provider protects 2–8°C by controlling “too warm” and “too cold.” Freeze damage can be silent: the product looks normal, but performance is compromised. Many freeze events come from coolant placement and operator variation, not outdoor temperature.
Your medical ice box provider should design the pack-out so it is hard to make a dangerous mistake. That usually means separators, spacing rules, and a layout that prevents coolant from touching the payload.
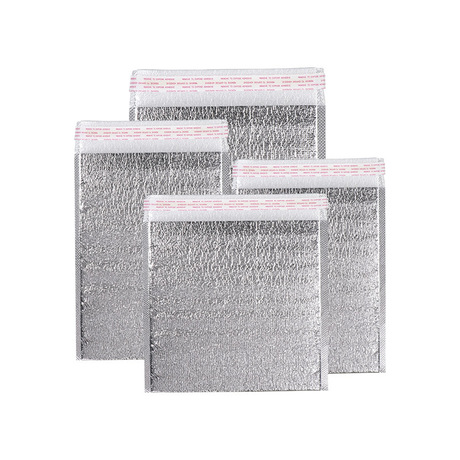
EPP vs EPS vs PU: what matters for you
| Material | Insulation stability | Reusability | What it means for you |
| EPS foam | Moderate | Low | Often single-use, simpler but less durable |
| EPP foam | High | High | Strong balance for repeat medical deliveries |
| PU foam | Very high | Medium | Often chosen for longer-duration lanes |
Pack-out guardrails that reduce freeze risk
No direct coolant contact: use separators or defined air gaps.
Pre-set layout: make “the right way” the easiest way.
Operator-proof steps: fewer decisions during busy shifts.
Example scenario: A regional program reduced excursions after switching to a pack-out that physically prevented coolant from touching vials. The system didn’t get “colder.” It got safer.
How can a medical ice box provider cut total cost without cutting safety?
A smart medical ice box provider lowers total cost by reducing errors, re-ships, and packing time. Unit price is not the whole story. One temperature excursion can erase months of packaging savings—especially when product value is high.
Total cost lives in hidden places: labor minutes, overpacked coolant weight, emergency freight, complaint handling, and disposal. A good medical ice box provider helps you remove waste from the system while keeping your temperature guardrails intact.
Where total cost usually hides
| Hidden cost area | What causes it | What to ask your provider | What it means for you |
| Overpacking coolant | No lane logic, fear of drift | “Can you design lane-based coolant plans?” | Lower weight and freight cost |
| Slow packing labor | Too many steps, unclear SOP | “Can we simplify to 3–5 steps?” | Higher throughput in peak season |
| Re-ships | Weak buffer or inconsistent builds | “What buffer time is validated?” | Fewer emergency shipments |
| Returns & disposal | No reuse plan | “Do you offer a reusable program?” | Lower waste, clearer handling |
Reusable vs single-use: choosing what fits you
| Model | Best-fit scenario | Common risk | What it means for you |
| Single-use | Low volume, unpredictable routes | Disposal cost and waste | Simple ops, higher material flow |
| Reusable | Stable lanes, high volume | Lost assets, return delays | Lower long-run cost if managed well |
| Hybrid | Mixed lanes and volumes | Planning complexity | Use reusables only where ROI is clear |
Practical tips you can use today
Right-size first, then optimize coolant. Empty air space can raise risk and cost.
Time your pack-out. If it takes too long, errors multiply under pressure.
Pilot reusables on one loop. Start with predictable facility-to-facility routes.
How does a medical ice box provider support compliance and audits in 2026?
A medical ice box provider supports compliance through documentation, traceability, and consistent manufacturing. In audits, “we think it works” is not enough. You need evidence you can store, retrieve, and explain—especially when shipments are high-value or high-risk.
Compliance is also about repeatability. Your provider should produce the same performance every time, across batches and sites. That means material traceability, defined inspection steps, and clear operating instructions that your team can follow.
A GDP-ready documentation checklist (buyer-friendly)
Ask your medical ice box provider for:
Quality process overview: how issues, deviations, and corrective actions are handled
Traceability basics: batch IDs for critical components and finished goods
Pack-out and handling SOPs: including training format and refresh cadence
Change control statement: what triggers re-test and how notice is given
Reusable cleaning guidance (if relevant): inspection, cleaning steps, rejection rules
Practical tips you can use today
Store validation files with shipment records. Make audits faster.
Standardize models across sites. Fewer SKUs means fewer training mistakes.
Train with visuals. A photo SOP beats a long paragraph every time.
How to shortlist a medical ice box provider in 15 minutes
Use this quick decision tool to compare candidates consistently.
Step 1: Pick your scenario
Scenario A: 2–8°C vaccines and refrigerated meds
Scenario B: lab samples with frequent handoffs
Scenario C: long-duration lanes with high delay risk
Scenario D: last-mile healthcare delivery with frequent openings
Step 2: Score 7 categories (0–5 each)
Validation proof (reports + conditions + curves)
Freeze-risk control (separators + layout guardrails)
Pack-out simplicity (fast, visual, low variation)
Documentation readiness (audit-friendly, consistent)
Scalability (capacity + consistency across batches)
Change control (written notice + re-test triggers)
Recovery support (what happens after an excursion)
Step 3: Interpret your total (max 35)
30–35: Excellent medical ice box provider for scale
24–29: Good medical ice box provider (lock guardrails in writing)
18–23: Pilot only (limit exposure)
<18: High risk (keep searching)
How do you run a pilot with a medical ice box provider without wasting months?
A good pilot proves repeatability under stress, not one perfect shipment. You want a process your team can repeat across operators, shifts, and delays. A structured pilot also prevents endless debating, because you define acceptance criteria up front.
A simple 5-week pilot plan
Week 1 — Lane definition: one lane, one product, one “worst-case” assumption
Week 2 — Configuration lock: pick 1–2 pack-outs and freeze the SOP
Weeks 3–4 — Controlled trial: ship with consistent packing and monitoring
Week 5 — Review: analyze drift, root causes, and operator variation
What to measure (keep it practical)
Percent of shipments within range
Packing deviations per 10 shipments
Packing time per unit
Damage rate
Response speed when exceptions occur
Preventing silent failure: how to monitor your medical ice box provider
Silent failure is when performance drifts without anyone noticing. Materials change, suppliers change, or assembly changes—yet the box looks the same. The result can be subtle: shorter hold time, sharper swings, or more operator sensitivity.
A disciplined medical ice box provider prevents this with change control and re-validation triggers. You can protect yourself with receiving checks and lane-level excursion tracking. This is not mistrust. It is basic risk management.
Quarterly provider health-check (yes/no)
Any unexplained excursions on stable lanes?
Any late deliveries during peak weeks?
Any reported material or design changes in the last 6 months?
Any packer confusion or repeated SOP mistakes?
Any rise in minor customer complaints?
Can the provider show batch traceability for current deliveries?
If you hit “yes” twice or more, take action: request a corrective plan and a re-validation review.
Practical tips you can use today
Build a receiving checklist: dimensions, closure integrity, labeling consistency.
Track issues by lane, not only by product. Lane signals appear earlier.
Write change notice into purchase terms. It’s your early warning system.
2026 medical ice box provider trends you should plan for
In 2026, buyers are pushing for systems that are easier to operate, easier to audit, and less wasteful. A modern medical ice box provider is expected to support lane-based qualification, clearer documentation, and faster training.
Latest developments you’ll see more often
Modular coolant kits: one box supports multiple hold times with controlled adjustments
Simplified SOP design: fewer steps, more visuals, fewer operator decisions
Reusable fleet programs: strongest fit for stable healthcare networks and lab loops
Stronger change control expectations: formal notice and retest triggers become standard
Operational proof over marketing: readable reports and clear assumptions win deals
Market insight (simple and actionable)
If your organization faces more audits and more cost pressure at the same time, prioritize providers that reduce labor and re-ships. A cheaper unit price is not a win if it increases packing errors or drift risk.
Common questions (FAQ)
Q1: What should a medical ice box provider include besides the container?
A medical ice box provider should include a coolant plan, a visual pack-out SOP, validation proof, and change control—so performance is repeatable.
Q2: How do I choose a medical ice box provider for 2–8°C shipping?
Start with lane time and add delay buffer. Then require configuration-specific validation reports and a pack-out your team can repeat quickly.
Q3: How long should a medical ice box provider hold temperature?
Many systems target 24–72 hours, while higher-risk lanes often plan 48–96 hours once buffer is included. Always confirm with proof.
Q4: Is a reusable medical ice box provider always cheaper?
Not always. Reuse wins when returns are predictable, cleaning is consistent, and loss rates stay low. Otherwise, hybrid programs work better.
Q5: What is the most common reason medical ice box systems fail?
Packing mistakes and unmanaged delays are common causes. A strong medical ice box provider reduces both with SOP design and buffer planning.
Q6: How many tests should I run before scaling?
Run enough shipments to capture variation: multiple operators plus at least one “worst-case” assumption for your lane, not just mild days.
Summary and recommendations
A reliable medical ice box provider protects more than products—it protects patients, operations, and compliance. Start with lane risk, then demand readable proof documents and a simple pack-out SOP. Control freeze risk with separators and layout guardrails, not “extra cold packs.” Finally, pilot on your toughest lane and lock change control into your purchasing terms. This approach reduces re-ships, lowers stress, and keeps audits calmer.
Next step (clear CTA)
Write down three facts: temperature band, lane duration, and worst-case delay. Then ask 2–3 medical ice box provider candidates for (1) a lane-matched configuration, (2) a photo SOP, and (3) a configuration-specific thermal report. If any provider cannot supply these, remove them from the shortlist.
About Tempk
Tempk supports medical cold chain teams with insulated shipping systems designed for real healthcare workflows. We focus on repeatable outcomes: simple pack-outs, consistent materials, and lane-based performance planning. Our goal is practical—help you reduce temperature excursions while keeping operations easy to train and easy to scale.
Call to action: Share your temperature band, expected transit time, and hottest ambient exposure. We’ll recommend a packaging approach you can validate and operate with confidence.