Pharmaceutical Cold Chain Transportation: How to Safely Deliver Medications in 2025
Pharmaceutical cold chain transportation ensures that vaccines, biologics and other temperature sensitive medicines reach you without losing potency. In 2025 this chain is more critical than ever – the global cold chain pharmaceuticals market is valued at about USD 6.67 billion and is projected to reach USD 9.71 billion by 2035. With roughly 16 billion injections administered annually and about 90 % occurring in curative care, keeping medicines within their prescribed temperature range protects both your health and the integrity of healthcare systems. This guide demystifies pharmaceutical cold chain transportation, explains why it matters, and shows you how to implement best practices.

What is pharmaceutical cold chain transportation and why does it matter? Learn why an unbroken chain from manufacturer to patient safeguards vaccines and biologics.
Which temperature ranges apply to different drug categories? Discover the critical ranges for vaccines, frozen biologics and ultra cold therapies.
How do packaging materials and monitoring devices work together? See how insulated containers, phase change materials and IoT sensors maintain conditions.
What regulations and best practices must you follow in 2025? Understand GDP, GMP and data integrity requirements.
Which sustainability and technological trends shape the cold chain? Explore reusable packaging, modal shifts and AI enabled monitoring.
What is pharmaceutical cold chain transportation and why is it critical?
In short: Pharmaceutical cold chain transportation is the end to end system that keeps medications at the right temperature from manufacturing to administration. It matters because many modern drugs – including vaccines, insulin, monoclonal antibodies and gene therapies – degrade if exposed to heat or freezing. When the cold chain fails, vaccines may lose efficacy, biologics can become toxic and expensive products must be discarded.
Why the cold chain matters for your health
Pharmaceutical cold chain logistics spans storage, handling, packaging, transportation and monitoring. Any deviation can compromise product integrity. Vaccines prevent about 4 million deaths per year and every dollar spent on immunization saves USD 52 in low and middle income countries. Yet the World Health Organization (WHO) estimates that up to 50 % of vaccines are wasted due to improper temperature control and logistics. For biologics, more than 85 % require cold chain management. This means failure isn’t just wasteful – it jeopardizes public health and drives up costs.
From a patient’s perspective, an unbroken cold chain means the medication you receive works as intended. Biologic drugs lose potency or become unsafe outside their range; vaccines exposed to freezing may require revaccination. Proper cold chain systems prevent such outcomes and ensure that therapies remain safe and effective.
The scope and growth of pharmaceutical cold chain logistics
The demand for temperature controlled medicines is booming. The global cold chain pharmaceuticals market is projected to grow from USD 6.67 billion in 2025 to USD 9.71 billion by 2035. This expansion is driven by the rise of biologics, gene therapies and vaccines, many of which need refrigerated (2 °C–8 °C), frozen (–25 °C to –15 °C) or ultra cold (–90 °C to –60 °C) conditions. Biologics now account for about one third of new drug approvals and over 85 % require cold chain support.
Cold chain failures have global implications. The WHO reports that nearly 50 % of vaccines are wasted each year due to poor temperature management. In low income countries, 1 in 5 children lacks access to life saving vaccines. Effective cold chain systems are essential to reduce waste, deliver new biologics and close the immunization gap.
How does pharmaceutical cold chain transportation maintain temperature ranges?
Core answer: Cold chain transportation maintains specific temperature ranges using specialized equipment, packaging and monitoring devices. Standard vaccines and refrigerated drugs typically require 2 °C–8 °C, frozen biologics need –25 °C to –15 °C, and ultra cold therapies such as mRNA vaccines require –90 °C to –60 °C. Controlled room temperature products are kept at 20 °C–25 °C.
Understanding temperature classes
In pharmaceutical logistics, temperature classes define how products are stored and transported:
Vaccines (standard): 2 °C–8 °C (36 °F–46 °F). Deviations lead to potency loss and revaccination.
Frozen biologics: –25 °C to –15 °C (–13 °F–5 °F). Warming causes structural damage and loss of efficacy.
Ultra cold biologics (e.g., mRNA vaccines, gene therapies): –90 °C to –60 °C (–130 °F– –76 °F). Even short exposure to warmth causes rapid degradation.
Room temperature drugs: 20 °C–25 °C (68 °F–77 °F). These still require climate control to avoid heat spikes.
Maintaining these ranges demands calibrated refrigeration units, cryogenic freezers and packaging designed to absorb or release heat at precise points. For example, the Pfizer BioNTech mRNA vaccine must be kept at –60 °C to –80 °C, while Moderna’s mRNA vaccine is stored at –20 °C.
Table: Typical temperature requirements
| Product category | Recommended range | Impact if breached | What it means for you |
| Vaccines (standard) | 2 °C–8 °C (36 °F–46 °F) | Potency loss; revaccination needed | Use dedicated vaccine refrigerators; avoid door openings |
| Frozen biologics | –25 °C to –15 °C (–13 °F–5 °F) | Structural damage; loss of efficacy | Invest in freezers designed for biologics; defrost regularly |
| Ultra cold biologics | –90 °C to –60 °C (–130 °F– –76 °F) | Rapid degradation if warmed | Use ultra cold freezers and cryogenic units; verify temperature probes |
| Room temperature medications | 20 °C–25 °C (68 °F–77 °F) | Potential potency loss; patient harm | Maintain climate controlled storage even for “room temperature” drugs |
Practical temperature control tips
Pre condition your equipment: Refrigerators and freezers should reach their target temperature before loading medicines.
Avoid overloading: Allow space around packages for air circulation; overloading creates warm pockets.
Label clearly: Mark shipments with required temperature ranges so carriers handle them correctly.
Educate customers: Inform patients to refrigerate medicines promptly upon delivery.
Real world case: A specialty pharmacy installed digital data loggers and remote alerts. During a summer heat wave, an alarm triggered when a refrigerator reached 9 °C; staff moved stock to a backup unit, saving over USD 50 000 in medication. Continuous monitoring prevented product loss and maintained patients’ therapy schedules.
Which packaging materials and technologies keep medicines safe?
Core answer: Effective packaging uses insulation, refrigerants and monitoring devices to maintain temperature throughout transit. Insulated containers made of expanded polystyrene (EPS), polyurethane (PUR) or vacuum insulated panels (VIP) form the outer shell, while gel packs, dry ice or phase change materials (PCMs) absorb or release heat. Data loggers or IoT sensors track temperature and provide proof of compliance.
Components of cold chain packaging
Pharmaceutical cold chain packaging is more than a box and ice packs. It consists of engineered layers:
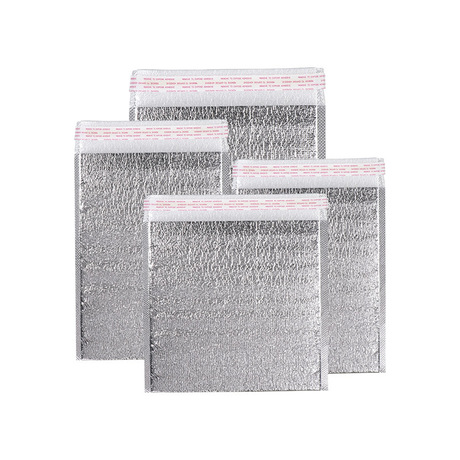
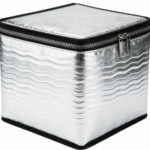
Insulated container: Typically made of EPS, PUR or VIP. It prevents external heat from entering and maintains internal stability.
Refrigerant: Gel packs, dry ice or PCMs. Gel packs absorb heat, dry ice sublimes at –78.5 °C, and PCMs maintain a specific temperature by absorbing or releasing latent heat.
Temperature monitoring: Data loggers or IoT sensors track temperature, humidity and location in real time. They provide early warning of excursions and documentation for regulators.
Protective outer packaging: Bubble wrap and outer cartons absorb shocks and protect labeling.
Choosing the right packaging
Your choice depends on product type, route and duration:
Match the temperature class: Vaccines require 2 °C–8 °C; some biologics need –20 °C or –80 °C. Always map your product portfolio to the correct thermal zone.
Consider transit duration: Long or complex routes may require VIPs, PCMs or portable freezers. Evaluate seasonal temperature swings and potential delays.
Validate packaging: Use pre qualified shippers and perform thermal modelling or performance testing to ensure the solution works in real world conditions.
Train your team: Many cold chain failures stem from human error. Ensure staff follow packing standard operating procedures and handle refrigerants safely.
Leverage redundancy: Maintain backup generators and extra refrigerants to prevent product loss during power outages or equipment failures.
Scenario: A rural clinic switched from household refrigerators to pharmaceutical grade units with VIP packaging and PCMs. Despite frequent power outages, the clinic maintained vaccine potency because VIPs held temperatures for days. Staff training on pack out procedures reduced errors.
How do IoT and monitoring technologies enhance cold chain reliability?
Core answer: Modern monitoring solutions combine sensors, data loggers, connectivity and analytics to track temperature, humidity and location throughout storage and transport. They provide real time alerts when temperatures drift and enable predictive maintenance and supply chain optimization.
Basic components and benefits
A cold chain monitoring system typically includes:
Sensors and data loggers: These small devices record temperature and sometimes humidity inside storage units or shipping containers. Basic loggers store data internally; advanced versions transmit data in real time.
Connectivity: Wireless technologies – Wi Fi, cellular, LoRaWAN, Bluetooth Low Energy (BLE) or RFID – transmit data to cloud platforms.
Cloud platforms: Software dashboards collect data, trigger alerts and provide analytics to help operators respond quickly.
Analytics and AI: Advanced systems analyze temperature trends, predict equipment failure and optimize logistics. For example, AI can forecast when a refrigerator might fail and schedule maintenance before a breakdown.
These components create a continuous “digital twin” of your cold chain, providing full visibility into every shipment. By automating temperature tracking, businesses can take corrective action immediately and reduce waste.
Monitoring technologies in practice
Data loggers: Compact, battery powered devices that record environmental conditions over time. They are affordable and easy to deploy but typically require manual data retrieval. Data loggers provide historical temperature records for compliance documentation.
IoT based wireless sensors: Sensors installed in storage or transport units transmit data continuously to cloud platforms via Wi Fi, cellular or LoRaWAN. They eliminate manual data collection and offer real time monitoring, enabling faster response to deviations.
RFID temperature sensors: RFID tags with temperature sensors are attached to pallets or packages; readers scan them at checkpoints. They streamline inventory management and automate data collection. However, they require infrastructure and have limited signal range.
GPS based trackers: These combine GPS location with temperature monitoring to provide visibility into the real time movement and condition of shipments. Alerts are sent if a shipment deviates from its planned route or experiences a temperature fluctuation.
Market growth and drivers
The global market for cold chain monitoring is expanding rapidly. Research estimates that the market, worth about USD 36.88 billion in 2024, will grow to USD 266.66 billion by 2034, with a CAGR of 21.88 %. Growth is fueled by stricter regulations, increased demand for temperature sensitive pharmaceuticals and the rise of e commerce. Regulations such as the FDA’s Good Distribution Practice (GDP) and European Medicines Agency guidelines mandate continuous temperature tracking and documentation, prompting companies to invest in monitoring technology.
Tip: When selecting a monitoring solution, consider connectivity coverage along your shipping route. Remote areas may require satellite or LoRaWAN sensors. Also assess data security and compliance with industry standards.
What regulations and best practices should you follow in 2025?
Core answer: Pharmaceutical cold chain transportation is governed by Good Distribution Practices (GDP), Good Manufacturing Practice (GMP), data integrity guidelines and country specific rules. These frameworks require accurate temperature maintenance, continuous monitoring, validated infrastructure and detailed record keeping. Failure to comply can lead to fines, product recalls and reputational damage.
Key regulatory frameworks
Good Distribution Practices (GDP): International standards covering every aspect of product distribution, emphasizing temperature control, validated systems, traceability and trained personnel.
NIST & UKAS Calibration: Calibration to standards like NIST (U.S.) or UKAS (U.K.) ensures measurement accuracy. Devices must have current calibration certificates.
EU GMP Annex 11 & Data Integrity Guidelines: These require validation of electronic systems, audit trails, secure access and reliable data handling.
EU Clinical Trials Regulation (EU) No 536/2014: Governs how investigational medicinal products are managed during trials, including temperature control and documentation.
Country specific rules: Agencies such as the U.S. Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA) publish additional guidelines.
The six principles of effective cold chain management
Temperature control & stability: Maintain stable conditions from production to administration using appropriate storage, transport and packaging.
Continuous monitoring: Use real time data and alert systems to respond to deviations immediately.
Traceable documentation: Maintain full records of temperature data, handling and deviations to demonstrate compliance.
Proactive risk management: Identify vulnerabilities and develop contingency plans.
Staff competency: Train everyone handling sensitive products to follow protocols.
Validated equipment & processes: Use tools and procedures tested to meet regulatory standards.
Consequences of cold chain failure
Cold chain breaches occur when products stray from their designated temperature range during storage or transit. Consequences include product degradation, public health risks, financial losses, regulatory action, reputational damage, supply disruptions and environmental waste. For many vaccines, even brief exposure outside 2 °C–8 °C can invalidate an entire batch.
Case study: During a distribution campaign, a logistics company failed to record continuous temperature data. Regulatory inspectors discovered gaps in the data and imposed fines. The company had to recall thousands of vaccine vials. Afterward, it implemented real time monitoring and staff training, reducing future excursions.
What sustainability trends and technological innovations are shaping the cold chain?
Core answer: 2025 sees a strong push toward sustainability and digital innovation. The industry is adopting reusable temperature controlled packaging, shifting from air to sea transport to reduce emissions, integrating AI and predictive analytics and embracing blockchain for traceability.
Reusable and sustainable packaging
Major pharmaceutical manufacturers are aiming for carbon neutrality by 2030. One key trend is the adoption of reusable temperature controlled packaging. Utilization rates are expected to rise from 30 % to 70 % in the coming years. Technological advances have made reusable solutions more affordable and efficient. Reverse logistics costs remain but are offset by overall cost effectiveness. Manufacturers and packaging providers collaborate to optimize designs, reducing waste and enhancing sustainability. Rental models allow companies to pay only for the duration of use and to scale up or down quickly.
Modal shift from air to sea
Switching transport modes can dramatically cut carbon emissions. Air freight generates 47 times more greenhouse gases per ton mile than ocean shipping. Cargo aircraft produce about 500 g of CO₂ per ton km, whereas cargo ships emit 10–40 g per ton km. Pharmaceutical companies are increasingly shipping by sea; some have more than 50 % of products moving via ocean, complemented by air transport when necessary. However, sea freight requires more inventory planning and reliable tracking systems.
Technology integration: AI, IoT and blockchain
AI and predictive analytics: Advanced monitoring systems use AI to forecast equipment failure, optimize route planning and identify patterns in temperature data. These insights help prevent excursions before they occur.
Internet of Things (IoT): Sensors, data loggers and GPS trackers provide real time visibility across multiple stages. Some solutions use LoRaWAN or Bluetooth Low Energy for remote areas, while others integrate with 5G networks.
Blockchain: For products such as vaccines, blockchain offers an immutable record of temperature, handling and chain of custody. This enhances transparency and trust, particularly for high value biologics.
Green energy and refrigerants
Sustainability efforts extend to refrigeration. Manufacturers are adopting natural refrigerants (such as CO₂ and hydrocarbons) with lower global warming potentials and exploring solar powered refrigeration units. Sustainable cold chain networks also emphasize energy efficient equipment and route optimization to minimize emissions.
2025 latest pharmaceutical cold chain developments and trends
Trend overview
2025 continues the momentum of vaccine distribution and biologics expansion. AI enabled monitoring, reusable packaging, modal shifts and stricter regulations shape the landscape. Governments and agencies are investing in cold chain infrastructure to support public health initiatives. For example, collaborations such as the 2025 Memorandum of Understanding between India’s National Accreditation Body for Cold Chain Management and Rwanda’s Foresight Institute aim to strengthen cold chain systems in Africa. In Asia, Indonesia is emerging as a regional hub for temperature sensitive pharmaceuticals due to increased exports and foreign investment.
Latest developments at a glance
Robotics and automation: Warehouses in Hong Kong are being transformed into state of the art cold chain facilities driven by robotics, improving safety and scalability.
International collaborations: Agreements such as the China–Cambodia “cold chain + general cargo” transport route enhance export capacity and improve temperature control.
Advanced packaging materials: Phase change materials and vacuum insulated panels are becoming standard for maintaining ultra cold conditions in shipping containers.
Cell and gene therapy logistics: These therapies require cryogenic storage (–150 °C or lower) and specialized chain of custody systems. CDMOs are expanding cryogenic capacity to meet this demand.
Monitoring market growth: The cold chain monitoring market is projected to expand at over 21 % CAGR between 2025 and 2034. This growth underscores the importance of technology investments.
Market insights
Pharmaceutical cold chain logistics is becoming a competitive differentiator. Companies that invest in integrated cold chain networks and digital monitoring are better positioned to deliver new therapies quickly and safely. The industry is seeing consolidation as logistics providers, packaging manufacturers and monitoring technology companies collaborate to offer end to end solutions. Regulations continue to tighten, requiring greater transparency and documentation.
FAQ: Frequently asked questions
Why do vaccines and biologics need cold chain transportation? Vaccines and biologics are complex molecules that degrade when exposed to temperatures outside their prescribed range. Exposure to heat or freezing can render vaccines ineffective or even dangerous.
What is a cold chain breach? A cold chain breach (or temperature excursion) occurs when a product strays from its designated temperature range during storage or transit. Even brief excursions can invalidate an entire batch of vaccines or biologics.
Which technologies help monitor the cold chain? Modern systems use data loggers, IoT sensors, RFID tags, GPS trackers and cloud platforms to monitor temperature, humidity and location in real time. AI algorithms analyze this data to predict equipment failure and optimize logistics.
How does reusable packaging improve sustainability? Reusable, temperature controlled packaging reduces waste and carbon emissions. Utilization rates are projected to rise from 30 % to 70 % in the coming years. Rental models allow companies to scale packaging as needed and avoid large capital investments.
What are Good Distribution Practices (GDP)? GDP encompasses international standards that govern the distribution of pharmaceuticals, requiring temperature control, validated systems, traceability and trained personnel.
Suggestion
Pharmaceutical cold chain transportation protects the efficacy and safety of temperature sensitive medicines. In 2025 the market is valued at around USD 6.67 billion and projected to grow steadily. Most vaccines and biologics require strict temperature ranges, from 2 °C–8 °C for standard vaccines to –90 °C to –60 °C for ultra cold therapies. Effective cold chain systems rely on engineered packaging, real time monitoring technologies, rigorous regulatory compliance and trained personnel. Sustainability trends such as reusable packaging and modal shifts from air to sea reduce emissions and costs. Continuous investment in digital monitoring, AI and infrastructure is essential to meet rising demand and ensure patient safety.
Actionable next steps
Assess your cold chain readiness: Map your product portfolio to temperature classes and identify high risk routes. Evaluate your packaging and monitoring systems for compliance with GDP and data integrity guidelines.
Implement real time monitoring: Invest in IoT sensors, data loggers and cloud platforms that provide real time alerts and analytics. Ensure devices are calibrated and certified.
Train your team: Develop standard operating procedures for packing, monitoring and emergency response. Conduct regular training and drills to prevent human error.
Adopt sustainable solutions: Explore reusable packaging and consider shifting appropriate shipments from air to sea to reduce your carbon footprint. Partner with providers offering rental models and regional expertise.
Stay updated with regulations: Monitor evolving guidelines from the FDA, EMA, WHO and local authorities. Maintain detailed records, calibration certificates and audit trails to demonstrate compliance.
By prioritizing cold chain integrity, you protect patient safety, reduce waste and position your organization for success in the evolving pharmaceutical landscape.
About Tempk
Company profile: Tempk specializes in developing innovative cold chain packaging and monitoring solutions for pharmaceuticals. Our products include insulated containers, phase change materials and digital data loggers designed to maintain precise temperature ranges. We leverage research and development to offer eco friendly, reusable packaging that meets stringent global standards. By combining advanced materials with real time monitoring technologies, we help clients safeguard their medicines, reduce waste and comply with regulations.
Call to action: To learn how Tempk can support your pharmaceutical cold chain transportation needs, contact our team for a customized consultation and explore solutions that ensure your products remain safe, effective and compliant throughout the journey.