Have you ever wondered why vaccines must stay cold, or how modern technology keeps them safe in transit? Vaccine cold chain trends have become a critical topic as more biologics and personalised medicines enter the market. Most vaccines need to remain between 2 °C and 8 °C, with frozen and ultra cold products requiring even lower temperatures. Yet up to 50 % of vaccines are wasted globally due to temperature excursions. As we move into 2025, a mix of market forces, innovative technologies and stricter regulations are reshaping how the cold chain works. This article breaks down the latest trends, explains why they matter for you and offers practical guidance to maintain vaccine integrity.

Why is the vaccine cold chain so important in 2025? – Learn how proper temperature control protects potency and saves lives.
What market forces and challenges shape vaccine cold chain trends? – Understand growth drivers such as biologics demand and why logistics can fail.
Which innovations are transforming the vaccine cold chain? – Explore how IoT sensors, blockchain, AI route optimisation and portable cryogenic freezers change logistics.
What are the best practices for vaccine storage and handling? – Get clear guidelines for refrigerators, freezers, ultra cold units and staff training.
What are the latest developments and future trends? – Discover market projections, sustainability initiatives and the shift to personalised medicine.
Why Does the Vaccine Cold Chain Matter in 2025?
Direct answer
Maintaining a robust vaccine cold chain is vital because many vaccines lose potency when exposed to temperatures outside their specified range. Most routine vaccines require refrigerated storage between +2 °C and +8 °C, while frozen vaccines such as varicella or zoster must stay between –50 °C and –15 °C. Cutting edge therapies like mRNA boosters and gene therapies demand ultra cold storage (–80 °C to –60 °C). Without consistent temperature control, vaccine ingredients degrade quickly, leading to wasted doses and compromised immunity.
Expanded explanation
In 2024 the World Health Organization (WHO) estimated that approximately half of vaccines are wasted globally due to exposure outside the recommended temperature range. This statistic underscores how easily a temperature excursion can ruin valuable doses, costing billions of dollars and undermining public trust. Maintaining a proper cold chain protects patients, reduces waste and supports vaccination campaigns. According to the CDC’s Vaccine Storage and Handling Toolkit, refrigerators should maintain 2 °C–8 °C, freezers –50 °C to –15 °C, and ultra cold freezers –90 °C to –60 °C. Devices with digital data loggers are recommended to track temperature continuously and provide alarms for out of range events. Regular monitoring and calibration help ensure vaccines remain potent from manufacturer to patient.
As the number of vaccines grows—ranging from COVID 19 boosters and malaria vaccines to personalised gene therapies—so do storage complexity and risk. The AAAHC reminds providers that live attenuated vaccines often require frozen conditions (–15 °C to –50 °C) while most others must stay refrigerated. Because mistakes can lead to revaccination or disease outbreaks, 2025’s cold chain trends emphasize real time monitoring, staff training and emergency planning.
Components and Temperature Ranges of the Vaccine Cold Chain
| Component | Typical temperature range | Role in the chain | Practical benefits |
| Refrigerated storage (influenza, tetanus, MMR) | +2 °C to +8 °C | Keeps most vaccines viable by preventing degradation | Easy to maintain with medical grade refrigerators; ideal for routine immunization clinics |
| Frozen storage (varicella, zoster) | –50 °C to –15 °C | Preserves live attenuated vaccines by slowing viral replication | Requires specialized freezers; protects vaccines during shipping and long term storage |
| Ultra cold storage (mRNA boosters, gene therapies) | –80 °C to –60 °C | Maintains stability of lipid nanoparticle based or cell therapies | Uses ultra cold freezers or portable cryogenic units; essential for cutting edge biologics |
| Portable cryogenic freezers | –80 °C to –150 °C | Used for transporting biologics and cell therapies | Offer real time temperature tracking and can operate in remote areas |
Practical tips and advice
Use certified medical grade refrigerators and freezers: Household units often have uneven temperatures; invest in purpose built equipment with alarms and air circulating fans.
Place vaccines in the center of shelves: Avoid storing doses near doors or vegetable bins where temperatures fluctuate.
Monitor temperatures twice daily: Document readings at start and end of each workday and use digital data loggers for continuous monitoring.
Real case: During a 2024 pilot program in India, a community health centre used IoT enabled vaccine carriers that monitored temperature and location in real time. When traffic delays caused external temperatures to reach 35 °C, the system automatically adjusted coolant settings and alerted staff. The vaccines arrived safely, avoiding costly waste.
What Market Forces and Challenges Shape Vaccine Cold Chain Trends?
Direct answer
The vaccine cold chain is expanding rapidly due to rising demand for biologics, mass vaccination campaigns and personalised medicines. Analysts estimate the global healthcare cold chain logistics market was about USD 18 billion in 2024 and could exceed USD 23 billion by 2033. This growth is driven by an explosion of biologics (projected to surpass USD 720 billion by 2030), expanded vaccine programmes for COVID 19, malaria and RSV, and increased clinical trials. However, challenges such as temperature excursions, traceability gaps, high energy costs and regulatory complexity create barriers.
Expanded explanation
Cold chain logistics once served a narrow segment of pharmaceuticals, but 2025 sees them as a cornerstone of healthcare. Eighty percent of vaccines must remain within a narrow temperature range, and distribution to remote areas can stress the system. This is particularly acute in low resource regions where power supply is unreliable. Market growth is compounded by the rise of home healthcare: patients receive medications at home, requiring last mile cold chain solutions. Meanwhile, gene and cell therapies—representing about 20 % of new drugs—must be stored at ultra cold temperatures.
On the other side of the ledger, operators face several obstacles. Temperature excursions destroy product potency and cost money; the International Air Transport Association (IATA) reports that nearly 20 % of temperature controlled shipments are compromised, and about 30 % experience delays. Traceability gaps hamper the ability to pinpoint where a breach occurred, while high energy and operational costs burden facilities with unstable electricity. Regulatory complexity arises because different countries enforce varied standards (Good Distribution Practice, IATA CEIV Pharma, EU GDP), requiring compliance across borders.
Market forces, challenges and solutions
| Market driver or challenge | Evidence | Practical impact | Solution |
| Rising demand for biologics and personalised medicine | Biologics market expected to exceed USD 720 billion by 2030 | More temperature sensitive therapies require ultra cold storage | Invest in ultra cold freezers, cryogenic packaging and training |
| Expanded vaccine programmes | Vaccination campaigns for COVID 19, malaria and RSV demand cold chain capacity; 80 % of vaccines need strict temperature control | Logistics networks must reach rural regions and maintain 2 °C–8 °C | Use portable solar powered fridges and insulated carriers |
| Clinical trials and personalised medicine | Gene and cell therapies often require –80 °C storage | Transporting trial samples and patient specific doses is complex | Use digital twins to simulate logistics and IoT sensors for real time data |
| E commerce and home healthcare growth | More patients receive medicines at home | Last mile delivery requires small, reliable cold boxes | Adopt compact, reusable packaging and temperature monitors |
| Temperature excursions and lack of traceability | IATA notes ~20 % of shipments are compromised | Loss of products and regulatory non compliance | Implement real time monitoring, blockchain for traceability |
| High energy costs and sustainability | Cold chain accounts for ~2 % of global CO₂ emissions | Rising operational costs and carbon footprints | Invest in solar powered storage and sustainable packaging |
| Regulatory complexity | Differing guidelines (GDP, IATA, EU GDP) require compliance | Risk of fines and shipment delays | Work with compliance experts and adopt standardised documentation |
Practical tips and recommendations
Map your storage systems: Before using new equipment, perform temperature mapping to identify hot and cold spots.
Train your team: Cold chain management relies on human expertise. Provide regular training to staff on handling and emergency procedures.
Use condition monitored packaging: Packaging with integrated sensors verifies that vaccines stayed within range without opening boxes.
Case example: Gavi estimates that 2.3 million children die each year due to lack of access to vaccines, with 18 million “zero dose” children missing vaccinations because of supply chain issues. Innovations like the Emvolio backpack—a portable refrigerator with IoT sensors and live tracking—help health workers deliver vaccines to remote villages while maintaining proper temperature.
How Do Innovations Transform Vaccine Cold Chain in 2025?
Direct answer
New technologies are revolutionizing the vaccine cold chain by providing real time visibility, predictive analytics and sustainable solutions. IoT enabled smart sensors continuously monitor temperature, humidity and location; blockchain records each step of the supply chain to prevent tampering; AI powered route optimisation reduces transit time and predicts temperature excursions; portable cryogenic freezers maintain ultra cold conditions for gene therapies; and solar powered storage units make cold chain logistics possible in regions with poor electricity. Together these innovations cut waste, improve compliance and expand access to vaccines.
Expanded explanation
The shift toward digital transformation is not optional—it’s crucial to meet the demands of personalised medicine and global distribution. IoT sensors alert operators when temperatures drift, enabling immediate corrective action. These devices, often embedded in shipments, also provide GPS tracking and can integrate with cloud platforms. Blockchain offers tamper proof records of temperature data and shipment history. Because each block is linked chronologically, manufacturers, logistics providers and health clinics all share the same trusted data.
Artificial intelligence enhances logistics by optimising routes based on traffic, weather and geography. AI combined with historical data can predict equipment failures or temperature excursions before they happen. The integration of digital twins—virtual replicas of physical systems—allows operators to simulate cold chain operations, plan capacity and test emergency scenarios without risking real inventory. The portable cryogenic freezer is a notable innovation: it maintains temperatures between –80 °C and –150 °C even in remote settings. These units often include real time tracking and warning systems, enabling safe delivery of vaccines and gene therapies to areas without reliable power.
Sustainability is another key driver. Solar powered cold storage units and sustainable packaging (reusable containers, biodegradable thermal wraps) reduce energy costs and carbon emissions. With cold chain logistics estimated to contribute roughly 2 % of global CO₂ emissions, adopting greener practices supports corporate social responsibility and regulatory compliance.
Key innovations and their benefits
| Innovation | Evidence | How it helps you |
| IoT enabled smart sensors | Devices send real time alerts when temperatures go out of range | Prevents spoilage by enabling quick corrective action; provides GPS tracking and continuous visibility |
| Blockchain for traceability | Transparent, tamper proof record of temperature data and shipment history | Builds trust among stakeholders; ensures compliance and simplifies recalls |
| AI powered route optimisation | AI analyses traffic and weather to optimise routes and predict risk | Reduces transit time and energy use; anticipates excursions before they occur |
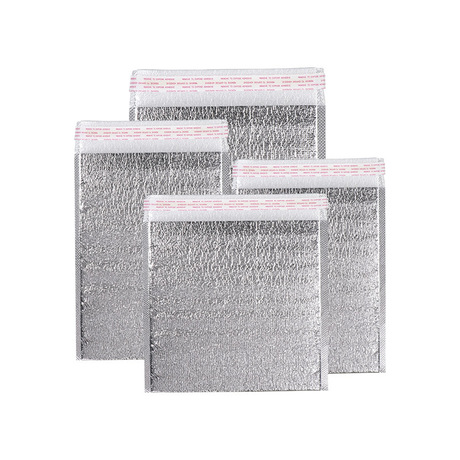
| Portable cryogenic freezers | Maintain –80 °C to –150 °C temperatures and provide real time tracking | Enables safe transport of gene therapies and biologics to remote locations |
| Solar powered storage units | Provide stable power in rural areas; energy costs 3.2–15.5 cents per kWh vs. 13.1 cents for grid electricity | Cuts energy costs; extends cold chain reach to areas without reliable electricity |
| Sustainable packaging | Recyclable and biodegradable thermal wraps reduce waste | Lowers environmental impact; meets regulatory and consumer demand for greener products |
| Digital twins and predictive analytics | Virtual models simulate cold chain operations and anticipate disruptions (citation from Tempk article) | Enables proactive planning; improves equipment maintenance and resource allocation |
Actionable tips for leveraging innovations
Integrate IoT sensors into every shipment: Choose sensors that track temperature, humidity and location and send alerts via SMS or email.
Adopt a blockchain platform: Work with logistics partners to implement blockchain for end to end traceability; this can reduce disputes and expedite audits.
Use AI for route planning: Feed live traffic and weather data into AI algorithms to determine optimal routes, reducing transit time and risk.
Invest in portable cryogenic freezers: If your organisation handles gene or cell therapies, portable units provide flexibility and compliance.
Example: A 2023 project in Southeast Asia used blockchain and IoT sensors to track vaccine shipments from factory to clinic. Real time temperature logs were shared among manufacturers, transporters and health clinics. When a sensor detected a temperature rise, the system triggered an alert, and the shipment was transferred to a backup freezer. No doses were lost, and regulatory reporting was simplified.
Best Practices for Vaccine Storage and Handling in 2025
Direct answer
Following evidence based storage and handling protocols is essential to protect vaccine potency and patient safety. According to the CDC, refrigerators must remain between +2 °C and +8 °C, freezers –50 °C to –15 °C, and ultra cold freezers –90 °C to –60 °C. Use digital data loggers with buffered probes to monitor temperatures and alarms to detect excursions. For 2024–2025 COVID 19 vaccines, the Pfizer BioNTech formula should be stored at –90 °C to –60 °C until expiration, then can be refrigerated for up to ten weeks. Always follow manufacturer instructions for each vaccine and maintain comprehensive documentation.
Expanded explanation
Best practices extend beyond temperature control. The CDC recommends using purpose built or pharmaceutical grade refrigerators and freezers because household units often have inconsistent temperatures and frost build up. Vaccines should be placed in the center of shelves, away from walls and doors, to ensure even airflow. Staff should check and document temperatures at least twice daily and maintain logs for three years. Digital data loggers provide detailed temperature histories and should be calibrated every two to three years.
Training is equally important. All staff members involved in vaccine handling must know how to store vaccines, recognise temperature excursions and follow emergency protocols. Clear Standard Operating Procedures (SOPs) should cover routine storage, transport, and emergency responses. Facilities must also prepare contingency plans for power outages or equipment failures and have backup storage options.
Practical tools to maintain cold chain integrity
| Tool or practice | Evidence | Benefit |
| Digital data logger (DDL) | CDC recommends DDLs for each storage unit and transport container | Provides accurate, continuous temperature records and alarms |
| Emergency SOPs and backup equipment | Facilities should have contingency plans and backup refrigerators | Prevents vaccine loss during power failures or mechanical issues |
| Staff training and documentation | AAAHC emphasises training on recognition of compromised vaccines and failure protocols | Ensures consistent handling and reduces risk of error |
| Manufacturer instructions | Some vaccines like Pfizer BioNTech require specific ultra cold storage followed by refrigerated thawing | Avoids inadvertent freezing or overheating of sensitive vaccines |
| Temperature mapping | Tempk article recommends mapping storage equipment before use | Identifies hot and cold spots and ensures uniform temperatures |
Additional tips
Do not use vegetable bins or refrigerator doors for vaccine storage, as temperatures fluctuate widely.
Label shelves and storage containers clearly to avoid mixing different vaccines and expiry dates.
Keep vaccines in their original packaging to protect them from light and maintain manufacturer specified conditions.
Regularly audit your processes. Review temperature logs and equipment maintenance records to identify patterns or recurring issues.
Practical example: The malaria vaccine rollout in 2024 used solar powered ice lined refrigerators that maintained proper temperatures for 115 hours under 43 °C ambient heat, exceeding WHO’s requirement of 72 hours. This allowed remote clinics to store vaccines safely and tripled the number of doses administered to children in some regions.
What Are the Latest Developments and Future Trends?
Trends overview
The vaccine cold chain industry is evolving quickly. Several 2025 trends will shape how vaccines are stored, transported and managed:
Surging biologics and personalised medicine: Gene and cell therapies require ultra cold storage, boosting demand for –80 °C to –150 °C equipment.
Modular and hyper local storage: Mobile and modular cold rooms allow vaccines to be stored closer to the point of use, enabling rapid response during outbreaks and reducing transit time.
Sustainability efforts: The global cold chain accounts for roughly 2 % of CO₂ emissions, prompting adoption of renewable energy, recyclable packaging and energy efficient refrigeration.
Digital transformation: End to end visibility with IoT, blockchain and AI is becoming standard. Predictive analytics and digital twins help organisations anticipate disruptions.
Regulatory harmonisation: International guidelines like GDP and IATA CEIV Pharma are aligning, making cross border operations smoother but requiring more rigorous documentation.
Automation and robotics: Approximately 80 % of warehouses are not yet automated. Adoption of automation, robotics and smart warehousing will accelerate to meet growing demand and reduce human error.
Latest progress at a glance
Real time tracking adoption: Hardware dominates more than 76 % of the cold chain tracking market, and 74 % of logistics data is expected to be standardised by 2025. This ensures more reliable data across the supply chain.
Growth of the pharmaceutical cold chain market: The global pharmaceutical cold chain market is forecast to reach USD 1,454 billion by 2029, growing at a compound annual growth rate (CAGR) of 4.71 %. This growth is fueled by cell and gene therapies, GLP 1 weight loss drugs and new vaccines.
Emergence of GLP 1 drugs: GLP 1 agonists used for obesity and diabetes must be stored at 2 °C–8 °C. Their popularity increases demand for reliable refrigeration even in retail pharmacies.
Market insights
Precedence Research reports that the global cold chain logistics market—including food and healthcare—was worth USD 436.30 billion in 2025 and is expected to reach USD 1,359.78 billion by 2034, expanding at a CAGR of around 13.46 %. Although healthcare represents a fraction of this market, the growth illustrates how cold chain logistics are becoming integral to global trade. Growth is particularly strong in the Asia Pacific region due to increasing vaccination programmes and investments in technology.
Frequently Asked Questions
Q1: What is the ideal temperature range for most vaccines?
Most vaccines should be stored between +2 °C and +8 °C to preserve potency. An ideal midpoint of +5 °C helps ensure stability. Use a medical grade refrigerator with a digital data logger for accuracy.
Q2: Which vaccines require ultra cold storage?
mRNA vaccines and many gene or cell therapies need ultra cold conditions, typically –80 °C to –60 °C. Portable cryogenic freezers can maintain temperatures as low as –150 °C for transport.
Q3: How long can the Pfizer BioNTech COVID 19 vaccine be refrigerated?
The 2024 2025 Pfizer BioNTech formula should stay in ultra cold storage (–90 °C to –60 °C) until expiration. After thawing, it can be refrigerated at 2 °C–8 °C for up to ten weeks. Once thawed, it must not be refrozen.
Q4: What percentage of vaccines are wasted due to cold chain failures?
WHO estimates that around 50 % of vaccines are wasted worldwide due to exposure outside recommended temperatures. Implementing real time monitoring, IoT sensors and proper staff training can significantly reduce waste.
Q5: How can I ensure my facility stays compliant with regulations?
Follow Good Distribution Practice (GDP), use calibrated digital data loggers, maintain accurate temperature logs for at least three years, and regularly review manufacturer guidelines. Conduct audits and staff training to ensure consistent adherence to SOPs.
Q6: What is the role of solar powered refrigeration in the vaccine cold chain?
Solar powered units provide reliable cold storage in areas with unstable electricity. They reduce operational costs—commercial solar rates are 3.2–15.5 cents per kWh, compared with 13.10 cents per kWh for grid electricity—and support vaccine distribution in rural communities.
Summary and Recommendations
In 2025, vaccine cold chain trends revolve around maintaining strict temperatures, expanding market demand and harnessing new technologies. The core temperature ranges—2 °C–8 °C for most vaccines, –50 °C to –15 °C for frozen products and –80 °C to –60 °C for ultra cold therapies—remain the foundation of cold chain management. The global healthcare cold chain market is growing rapidly due to biologics, personalised medicine and expanded vaccination campaigns. Innovations like IoT sensors, blockchain, AI powered route optimisation, portable cryogenic freezers and solar powered storage are transforming logistics and reducing waste. Yet challenges such as temperature excursions, traceability gaps, high energy costs and regulatory complexity persist.
Actionable next steps:
Audit and upgrade equipment: Ensure your facility uses purpose built refrigerators and freezers capable of maintaining appropriate ranges, and calibrate devices regularly.
Implement real time monitoring and blockchain: Adopt IoT sensors with GPS and use blockchain to record temperature data and improve transparency.
Train your team and document everything: Provide regular training on storage procedures, emergency responses and documentation. Maintain digital logs for at least three years.
Plan for contingencies: Develop SOPs for power outages, equipment failure and transport delays. Maintain backup refrigeration and transport containers.
Invest in sustainability: Explore solar powered refrigeration and sustainable packaging to cut energy costs and reduce your carbon footprint.
Following these steps will help ensure vaccine integrity, reduce wastage and meet regulatory requirements.
About Tempk
Tempk is a leader in cold chain solutions for pharmaceuticals and biologics. We specialise in high performance insulated packaging, advanced data loggers and renewable powered refrigeration systems. Our products are designed to keep vaccines and biologics within their required temperature ranges, from +2 °C to –150 °C, while offering ease of use and cost efficiency. With our R&D centre focused on innovation and sustainability, we provide solutions like 0–10 °C insulated boxes, solar powered coolers and IoT enabled tracking devices that help healthcare organisations maintain compliance and reduce waste.
Call to action
Ready to enhance your vaccine cold chain? Contact Tempk’s specialists for a personalised assessment and discover how our data driven packaging and real time monitoring solutions can safeguard your products and support your sustainability goals.