What Is Cold‑Chain Clinical Specimens? Understanding Critical Temperature Control
Cold‑chain clinical specimens are biological samples that must be kept within controlled temperatures throughout collection, storage, transport, and testing. In 2025, temperature maintenance is more important than ever in diagnostics, research, and patient care. Proper cold‑chain handling preserves sample quality and ensures accurate results. Without it, tests can fail and patient outcomes can worsen.
This article will help you understand:
-
What cold‑chain clinical specimens are and why they matter, including key temperature ranges.
-
How cold chain is managed step by step to prevent sample degradation.
-
Best practices for transport and logistics for labs, clinics, and research sites.
-
Common mistakes and how to avoid them in sample handling.
-
Latest trends and 2025 industry insights on cold‑chain bio‑specimens.
What Are Cold‑Chain Clinical Specimens and Why Do They Matter?
Cold‑chain clinical specimens are biological samples that must be kept within strict temperature limits from the moment of collection until laboratory analysis. These include blood, tissue, swabs, DNA/RNA samples, sputum, and more. If temperatures vary outside these narrow bands, the sample can degrade, leading to inaccurate results or unusable data.
Maintaining this cold chain is not optional—it preserves sample integrity and ensures that diagnostic tests reflect reality. For instance, many molecular tests rely on intact RNA and DNA. If those molecules break down due to heat exposure, test sensitivity drops sharply.
Why Temperature Matters for Clinical Specimens
Temperature determines how quickly biological molecules break down or how microorganisms change. For most cold‑chain clinical specimens:
-
Refrigerated range (2°C–8°C) is common for blood and many diagnostic kits.
-
Frozen (−20°C) and ultra‑cold (≤−80°C) conditions support long‑term storage, especially for cell cultures and gene therapy samples.
If cold chain breaks—even briefly—enzymes like RNases can degrade nucleic acids, invalidating test results. This leads to false negatives, repeated sampling, increased costs, and delayed care.
How Does Cold Chain Work for Clinical Specimens?
Cold chain for clinical specimens is an unbroken temperature‑controlled process that includes:
-
Collection
-
Temporary storage
-
Packaging and logistics
-
Transport and monitoring
-
Laboratory receipt and testing
Each step must be meticulously planned and executed.
How Are Clinical Specimens Collected and Stored Initially?
Correct collection and immediate storage set the foundation for cold‑chain integrity. Specimens are collected following strict protocols to avoid contamination and temperature stress.
-
Collection devices like swabs and tubes must be pre‑conditioned if needed.
-
Samples often go directly into refrigerated (2°C–8°C) or frozen storage (± specific target).
-
Controls such as temperature‑label indicators ensure samples start their journey within range.
Proper initial handling prevents early degradation and sets baseline quality for downstream processes.
H3: Tools and Containers Used at Collection
Clinical collection sites use verified containers and media designed to preserve temperature and protect sample chemistry:
| Tool | Use | Key Benefit |
|---|---|---|
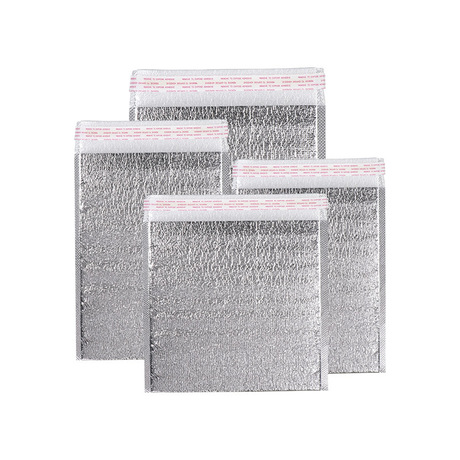
| Insulated thermo‑packs | Stabilize refrigerated conditions | Maintains 2–8°C during first hours |
| Ultra‑cold containers | Dry ice or phase change materials | Supports ≤−80°C for critical samples |
| Data loggers | Continuous temperature tracking | Detects deviations in real‑time |
Even with sound tools, human handling mistakes—like leaving tubes at room temp—can break the cold chain before it even begins.
What Temperature Ranges Are Required for Different Samples?
Cold‑chain requirements vary by specimen type and test method. Below are typical target ranges:
-
Refrigerated (2°C–8°C): Blood analytes, serology kits.
-
Frozen (−20°C): Some viral components, DNA samples.
-
Ultra‑cold (≤−80°C): Cell cultures, gene therapy, long‑term storage.
How Temperature Affects Sample Integrity
Temperature excursions can:
-
Cause denaturation of proteins.
-
Reduce nucleic acid stability.
-
Lower sensitivity of molecular tests.
-
Increase false negatives or ambiguous results.
In practical terms, an RNA sample exposed even briefly to 15°C can lose enough integrity that polymerase chain reaction (PCR) tests return compromised data.
How Are Cold‑Chain Clinical Specimens Packaged and Transported?
H2: What Are the Key Packaging Techniques in 2025?
Cold‑chain packaging ensures the specimen stays within its required temperature zone throughout transit:
-
Insulated boxes with phase change materials maintain temperature for hours or days.
-
Dry ice or ultra‑cold materials are used for deep‑freeze specimens.
-
Real‑time IoT sensors track temperature, humidity, and shock. FedEx
Packaging is validated—tested to confirm that it holds temperatures for the expected transit duration.
Step‑by‑Step Packaging Process
-
Condition cold packs/dry ice to proper temperature before loading.
-
Place specimen in primary leakproof container with absorbent.
-
Add secondary insulation and temperature‑stabilizing materials.
-
Include data logger or sensor tag to record environmental conditions.
-
Seal and label according to biohazard and cold‑chain standards.
A common mistake is misjudging the transit time and ambient temperature, especially in summer months or long distances.
Transport Modes and Monitoring
Transport can be by ground, air, or express logistics, depending on urgency. Throughout:
-
GPS monitoring tracks location.
-
Temperature monitors send alerts if excursions occur.
-
Backup plans like regional cold storage hubs protect high‑value samples.
What Happens at the Laboratory Receipt?
When specimens reach the laboratory:
-
Packing is inspected for seal integrity.
-
Temperature loggers are downloaded to confirm continuous compliance.
-
Specimens are immediately processed or stored at appropriate conditions.
Any evidence that the cold chain was compromised usually invalidates the specimen, requiring recollection.
Common Challenges and How to Overcome Them
Maintaining an unbroken cold chain for clinical specimens is complex. Here are common issues and solutions:
Challenge 1 – Temperature Excursions
Temperature excursions occur when specimens stray outside their required range. This can destroy sample integrity quickly.
Solution: Use real‑time monitoring and alerts so you can intervene before irreversible damage occurs.
Challenge 2 – Inaccurate Duration Estimates
Underestimating transit time—especially in remote regions—leads to cold chain failures.
Solution: Validate packaging holds beyond expected time frames and add buffer capacity.
Challenge 3 – Regulatory Compliance
Clinical specimens are subject to rigorous shipping standards (e.g., biohazard labeling, GDP). Lack of compliance can delay transport or lead to fines.
Solution: Train staff thoroughly and use pre‑built compliance checklists for routine shipments.
2025 Trends in Cold‑Chain Clinical Specimen Handling
The industry is innovating rapidly. Here’s what you should know for 2025:
-
AI‑driven route optimization improves delivery precision.
-
Blockchain traceability enhances sample provenance and audit trails.
-
Eco‑friendly thermal materials reduce environmental impact.
-
Direct‑to‑patient lab drops reduce time and improve patient experience.
Latest Progress Highlights
-
Advanced IoT monitoring systems now integrate humidity, shock, and tilt detection.
-
Decentralised logistics allow clinical specimens to go from home collection to lab directly.
-
Predictive maintenance of refrigeration units reduces unplanned failures.
Best Practices Checklist for Cold‑Chain Clinical Specimens
-
Know your specimen temperature needs before collection.
-
Use validated packaging and pre‑conditioned materials.
-
Monitor in real time, with automated alerts.
-
Document every step—from collection to lab receipt.
-
Train personnel regularly on updated 2025 regulations.
FAQ – Cold‑Chain Clinical Specimens
What makes a specimen a cold‑chain specimen?
A specimen that must stay within a specific temperature range from collection to analysis to remain viable. It’s critical for accurate diagnostics.
Can clinical specimens be shipped without cold chain?
Generally no. Some specialised media can tolerate ambient conditions, but most diagnostic samples need controlled temperatures for valid results.
How long can specimens stay in cold chain packaging?
Advanced packaging can maintain required temperatures for 48–96+ hours, depending on materials and ambient conditions.
What if a cold‑chain breach happens?
Immediate documentation, review of temperature logs, and often recollection of the sample are necessary.
Summary and Final Advice
Cold‑chain clinical specimens are temperature‑sensitive biological samples that require an unbroken controlled environment from collection to testing. Keeping them within required temperature ranges preserves sample quality and ensures reliable results. Key strategies include validated packaging, real‑time monitoring, regulatory compliance, and ongoing training.
Take action:
-
Audit your current cold‑chain processes.
-
Implement real‑time sensors and buffer packaging.
-
Train teams on 2025 standards and best practices.
By taking these steps, you protect valuable specimens, reduce waste, and support better patient outcomes.
About Tempk
At Tempk, we specialize in cold‑chain solutions for clinical and life science specimens. We focus on real‑time monitoring, validated temperature preservation systems, and expert support. Our systems help you maintain sample integrity, meet regulatory standards, and reduce risk across the cold chain.
Next Step: Contact us for a consultation tailored to your clinical logistics needs.